Table of Contents
- Summary
- What is Endometriosis?
- Estrogen and Endometriosis
- The Effects of Endometriosis
- Symptoms of Endometriosis
- Diagnosis of Endometriosis
- Taking Charge of Your Journey to Wellness
Summary:
- Endometriosis is a condition where tissue similar to the uterine lining grows outside the uterus, affecting 1 in 10 women in Canada.
- Estrogen drives the growth of endometriosis implants, causing them to swell, bleed, and trigger pain through inflammation.
- Symptoms vary by individual and implant location, commonly including painful periods, painful intercourse, bowel or urinary pain, infertility, and chronic pelvic pain.
- Diagnosis typically involves assessing symptoms, history, and imaging, but surgery remains the most reliable method for confirming endometriosis.
Endometriosis affects 1 in 10 women in Canada, and can have a devastating effect on daily life, often going unchecked for decades.
This condition involves tissue similar to the uterine lining growing outside the uterus, and can cause symptoms like painful periods and infertility. Estrogen promotes the growth of endometriosis implants, triggering pain and localized inflammation.
Diagnosis, typically made between ages 35 and 44, combines symptoms, exams, and surgical biopsy for confirmation, as no single test is definitive.
What is Endometriosis?
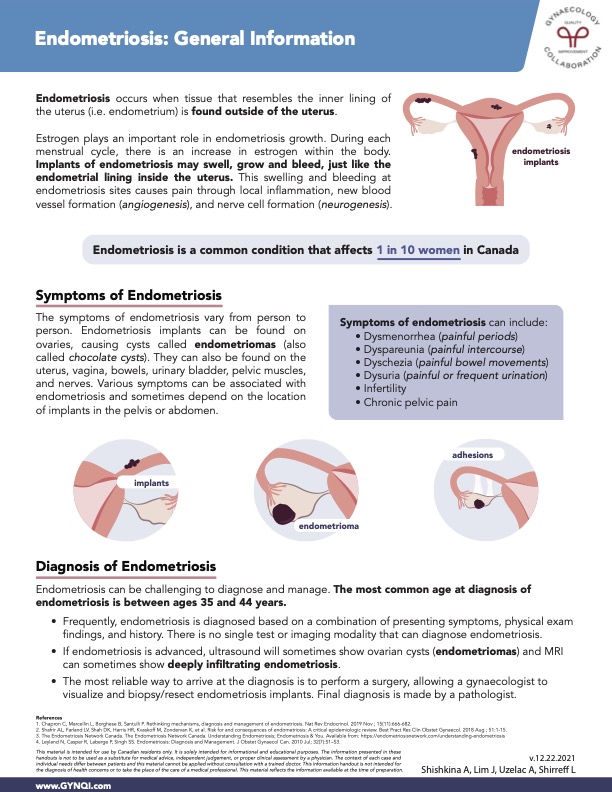
Endometriosis is a common condition that affects 1 in 10 women in Canada. It occurs when tissue similar to the inner lining of the uterus (the endometrium) grows outside the uterus.
Estrogen and Endometriosis
Estrogen plays a crucial role in the growth of endometriosis. During each menstrual cycle, estrogen levels rise, which can lead to swelling, growth, and bleeding of endometriosis implants, similar to the endometrial lining within the uterus.
This swelling and bleeding can trigger pain through local inflammation, the formation of new blood vessels (angiogenesis), and the development of nerve cells (neurogenesis).
The Effects of Endometriosis
The experience of living with endometriosis varies from person to person and can depend on the location of the implants. Endometriosis can cause cysts known as endometriomas (or chocolate cysts) when implants are found on the ovaries.
Various symptoms can be associated with endometriosis depending on the location of the implants in the pelvis or abdomen. Areas affected can include:
- Uterus
- Vagina
- Bowels
- Urinary bladder
- Pelvic muscles
- Nerves
Symptoms of Endometriosis
The symptoms of endometriosis can be diverse and vary widely among individuals, and depend on the locations where the endometrial implants are found.
Symptoms can include:
- Dysmenorrhea (painful periods)
- Dyspareunia (painful intercourse)
- Dyschezia (painful bowel movements)
- Dysuria (painful or frequent urination)
- Infertility
- Chronic pelvic pain
Diagnosis of Endometriosis
Diagnosing and managing endometriosis can be challenging, with the most common age of diagnosis typically occurring between 35 and 44 years.
- Endometriosis is often diagnosed through a combination of presenting symptoms, physical exam findings, and medical history, as there is no single test or imaging method that can definitively diagnose the condition.
- In advanced cases of endometriosis, ultrasound may reveal ovarian cysts known as endometriomas, while MRI can occasionally detect deeply infiltrating endometriosis.
- The most reliable method for diagnosing endometriosis is through surgery, which allows a gynecologist to visualize and biopsy or resect the endometriosis implants. The final diagnosis is confirmed by a pathologist.
It is important to discuss your treatment options with your doctor and healthcare team.
Taking Charge of Your Journey to Wellness
Endometriosis affects 1 in 10 women in Canada, and is characterized by tissue similar to the uterine lining growing outside the uterus. Estrogen drives the growth of these implants, resulting in pain and inflammation. Symptoms, which can include painful periods, intercourse, bowel movements, and infertility, vary depending on the implant locations. Proper diagnosis relies on symptoms, ultrasound, and surgical biopsy, as there is no definitive test.
Advocate for your health and speak to your healthcare professional to find a treatment plan that works for you.



