Navigating Hormone Therapy
There are different types of hormone therapy for perimenopausal and menopausal people. Whether you are a candidate for hormone therapy will depend on your symptoms, personal preferences and past medical and family history.
What to Expect with Hormone Therapy
In Canada, there are several reasons why doctors may suggest hormone therapy:
- Bothersome vasomotor symptoms
- Prevention and treatment of bone loss
- Prevention of conditions linked to low estrogen associated with early or premature menopause
- Genitourinary Symptoms
- Mood and sleep concerns, in selected cases
You may experience benefits from hormone therapy that do not appear on the list above. For example, you may see a positive change in your skin or nails, however, concerns related to either wouldn’t be the main reason your doctor is prescribing hormone therapy.
Exploring the information in the links below will allow you to learn more about different menopausal hormone therapies, their uses and some of the many products available in Canada.

Local Hormone Therapy
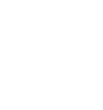
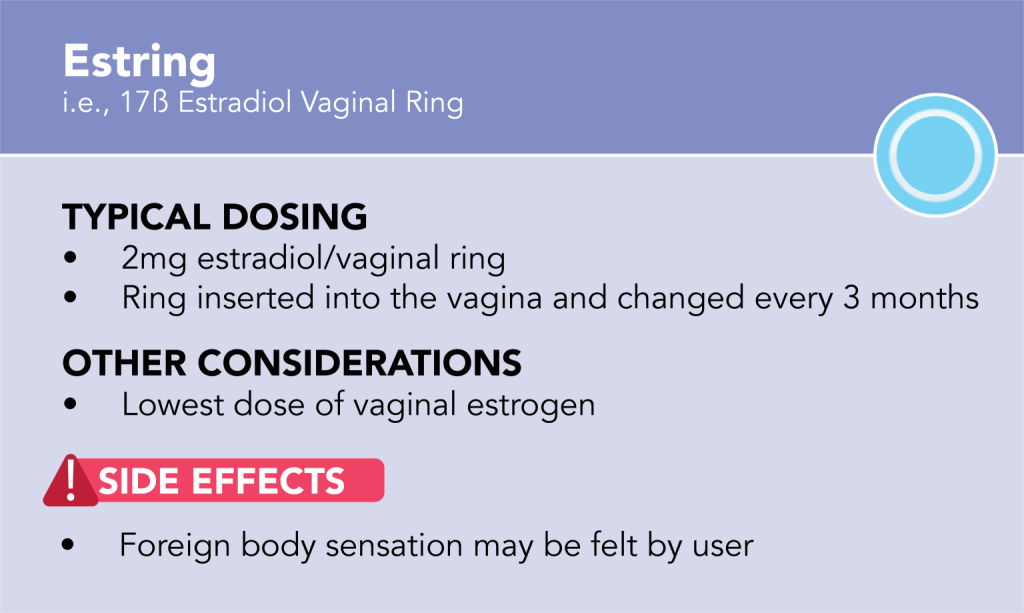
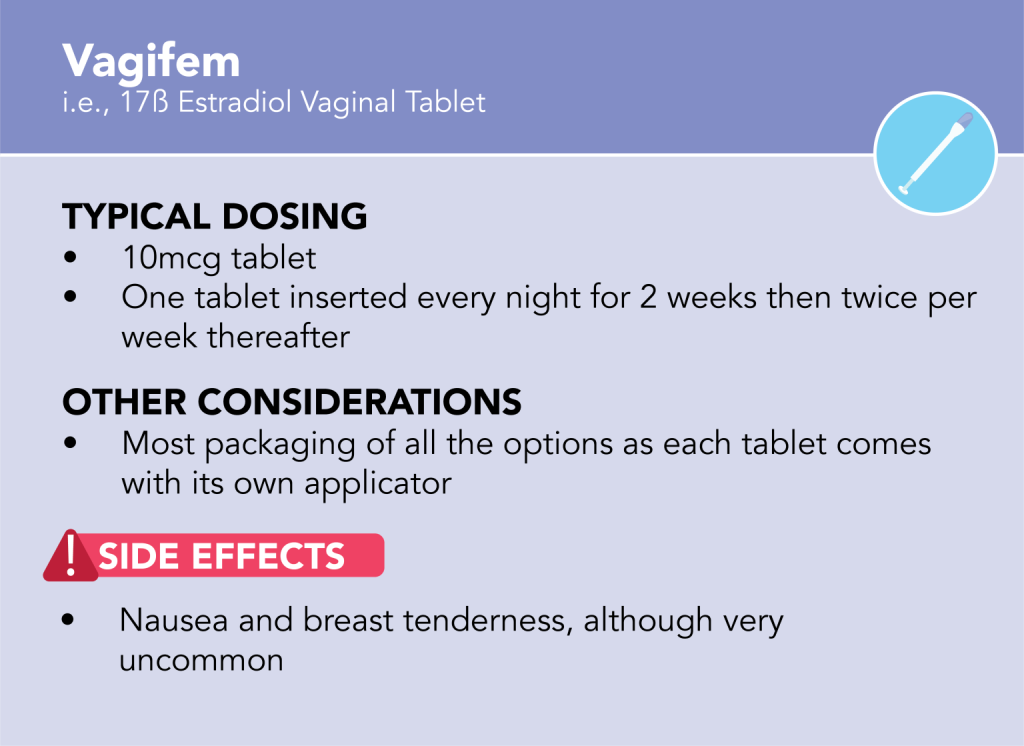
Local hormone therapy doesn’t carry the same risks as systemic hormone therapy. It is typically used to treat genitourinary (i.e., vaginal and/or urinary) symptoms.
Explore the links below to learn about different local hormone therapy products available in Canada.
While there are very few risks with these medications and most people are able to use these products safely, speak to your doctor about whether these options are right for you.

Video Resources
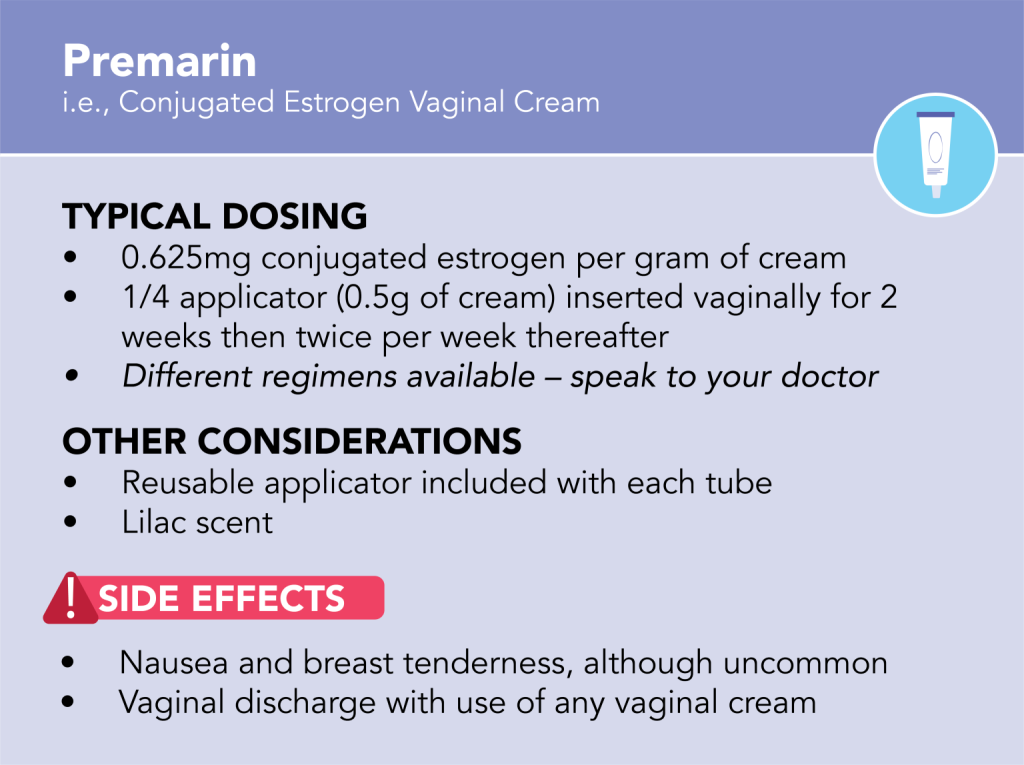
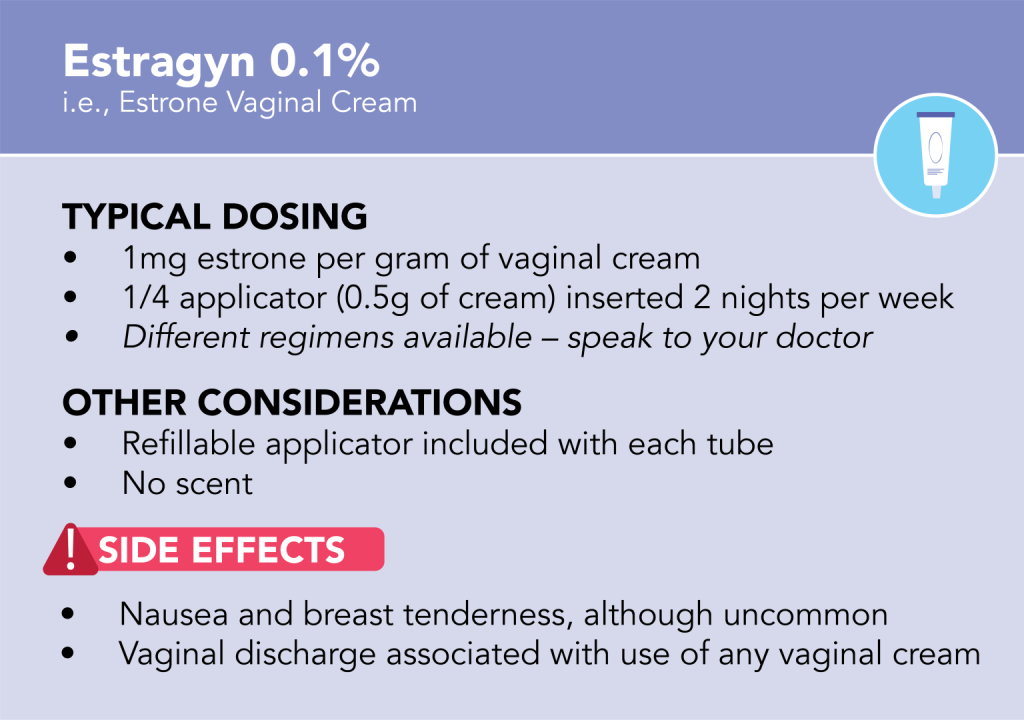
Common Local Hormone Therapy Products (Available in Canada)
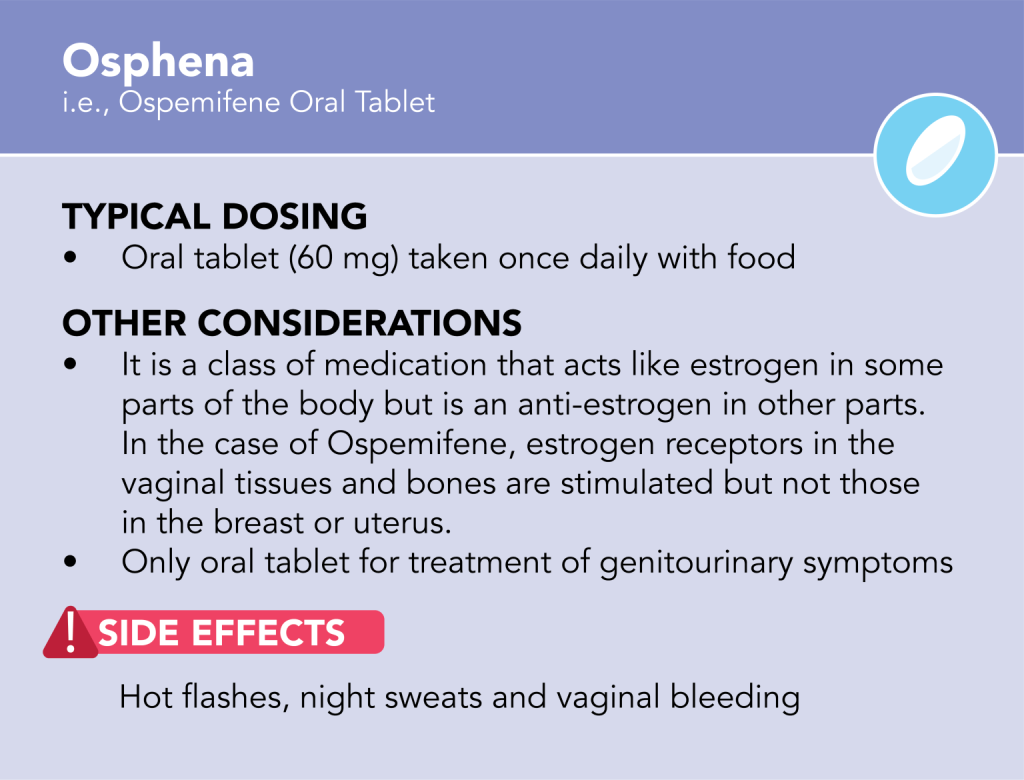
**Ospemifene (Brand Name: Osphena) is an oral tablet offering localized treatment. It carries more risk than local hormone therapy products. Speak to your doctor about whether it is right for you.
Handouts
Systemic Hormone Therapy
Systemic Menopausal Hormone Therapy (MHT) implies “whole body” exposure to the medication. This, therefore, can come with “whole body” benefits and risks, which don’t necessarily apply when someone uses local hormone therapy. Review our handouts below and click here to learn more about risks of systemic MHT. Some people should not take systemic MHT. Click here to learn more.
Different hormones can be prescribed for menopausal symptoms. These include estrogen, progesterone and testosterone. The two most commonly prescribed systemic hormones are estrogen and progesterone. For more information on testosterone therapy, please click here.

Estrogen

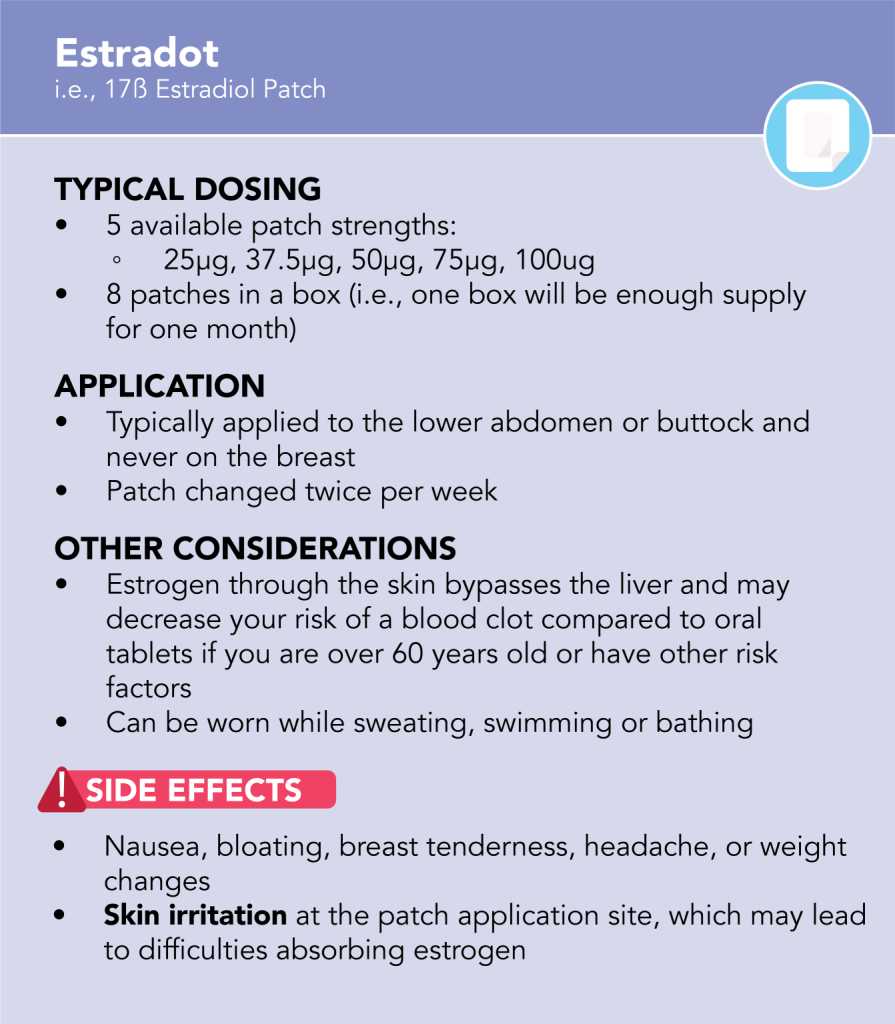
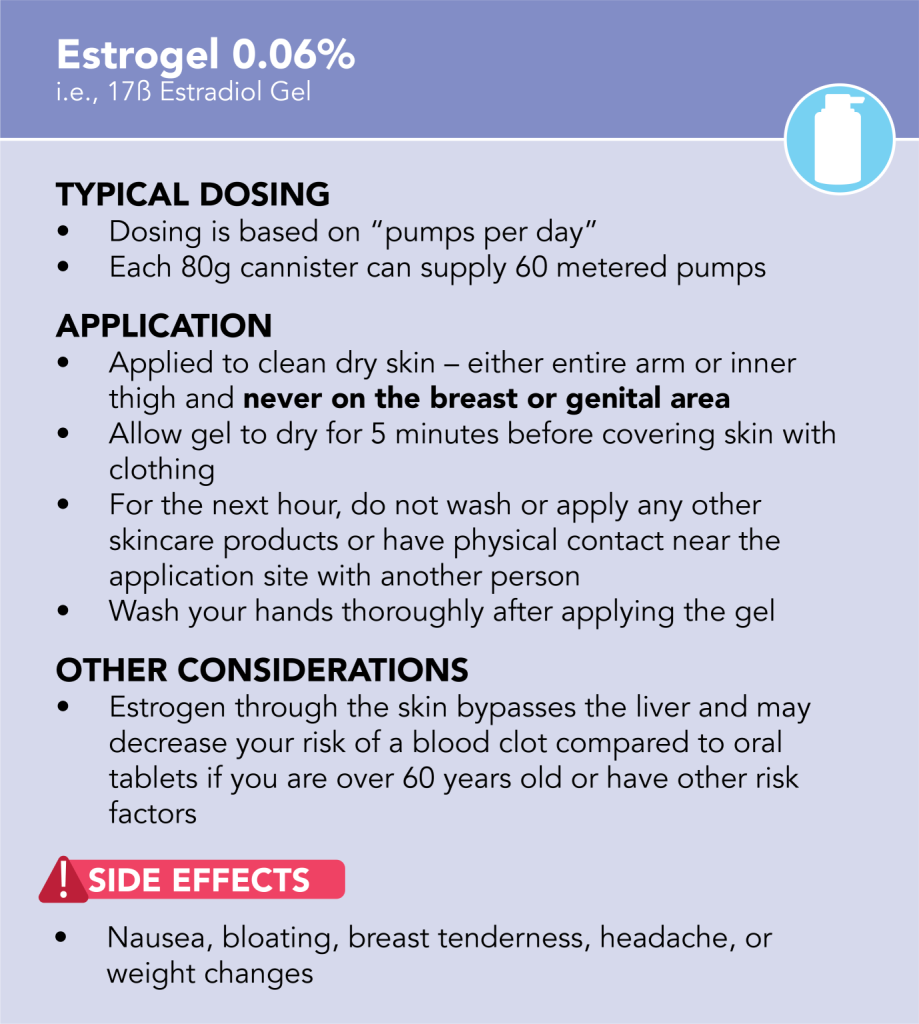
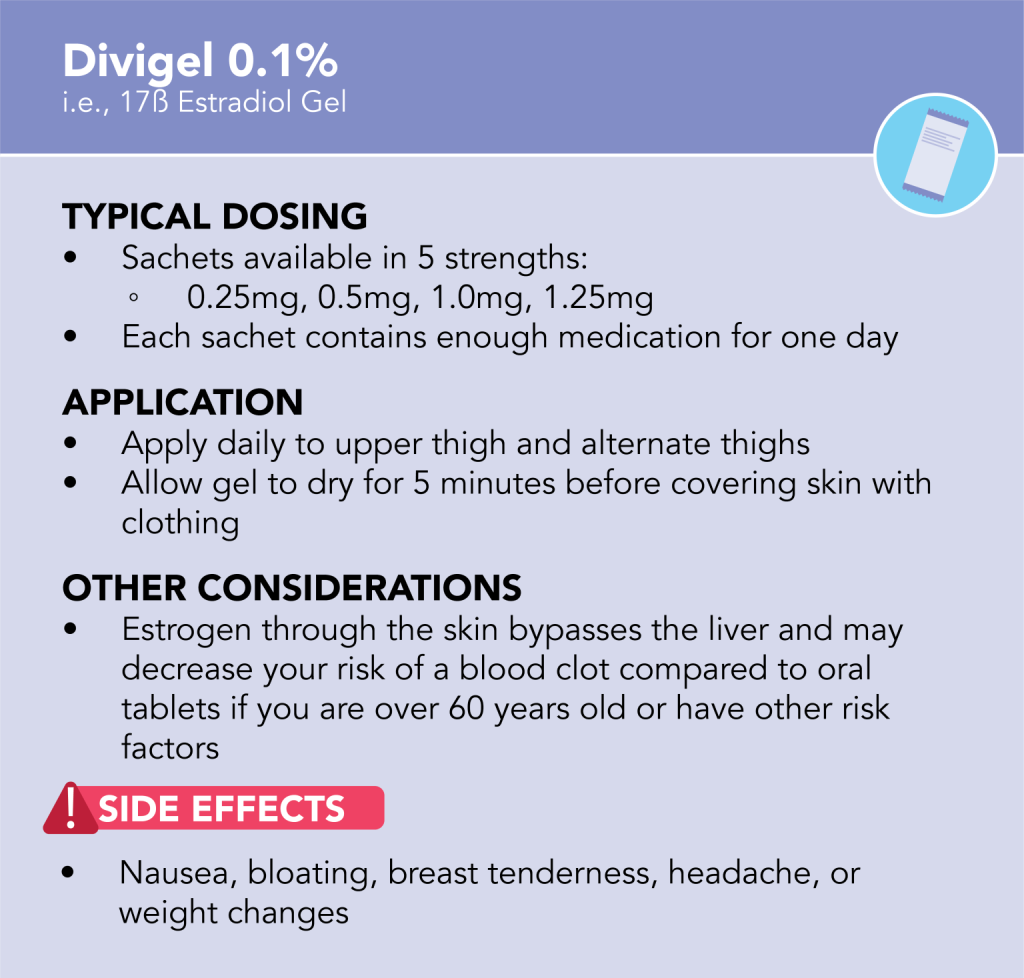
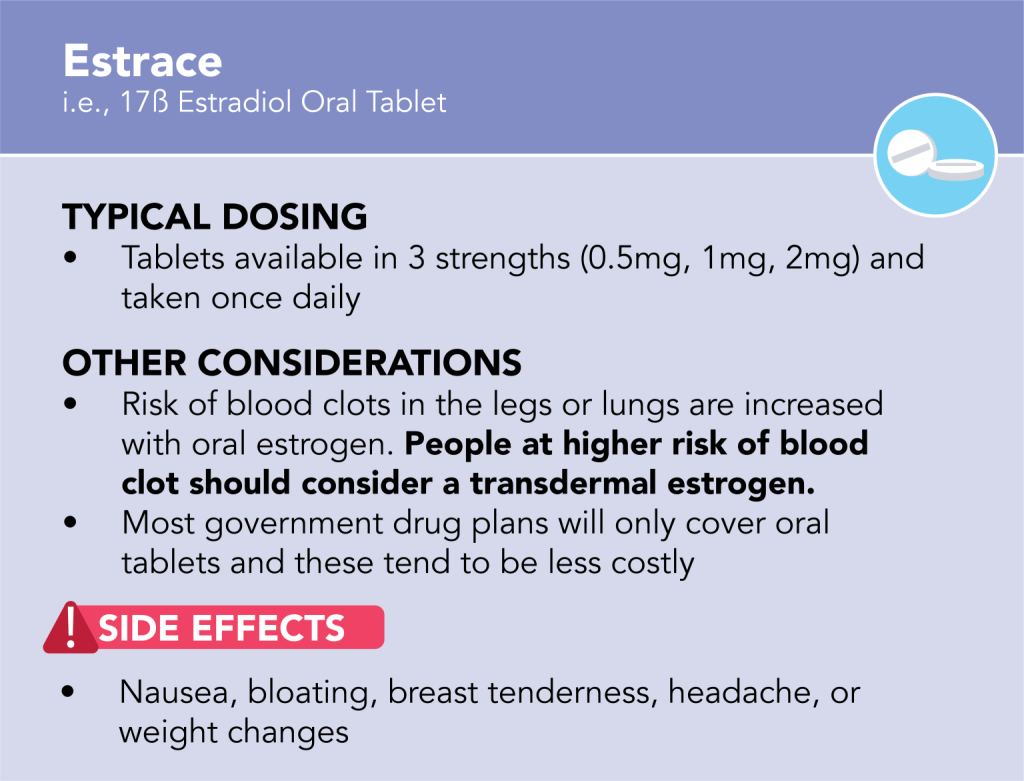
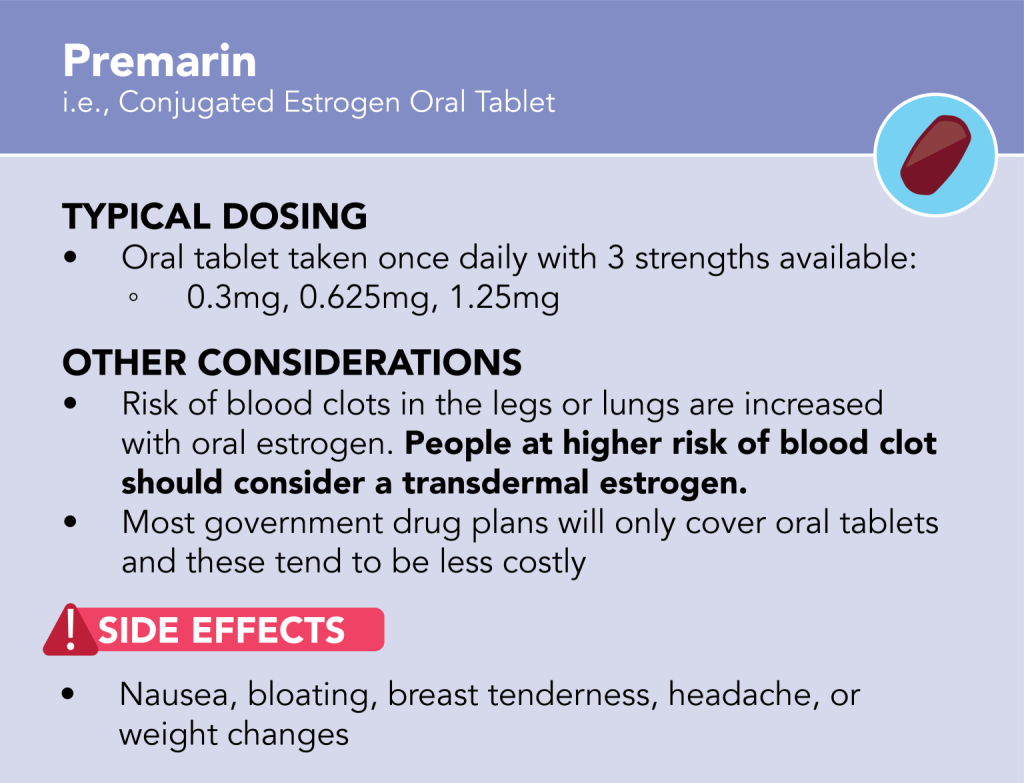
Estrogen can be given through the skin (transdermal administration) or by tablets taken by mouth (oral administration). Replacing your estrogen is the component of menopausal hormone therapy (MHT) that typically makes you “feel better” because many symptoms of menopause are due to low estrogen.
Progesterone

Progesterone can be given alone to treat some menopausal symptoms but isn’t typically as effective as estrogen. More commonly, progesterone is used to protect the lining of the uterus from developing cancer or precancer cells in people with a uterus who are prescribed and are prescribed a stand-alone estrogen.
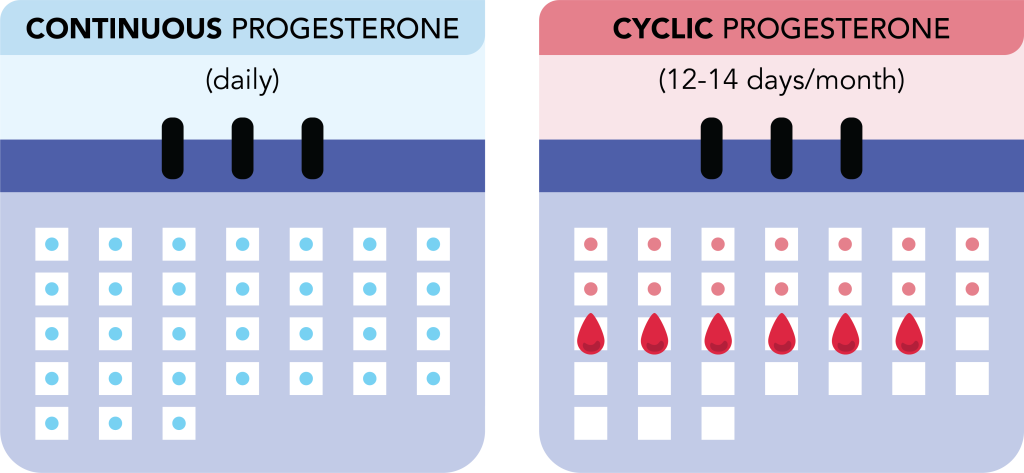
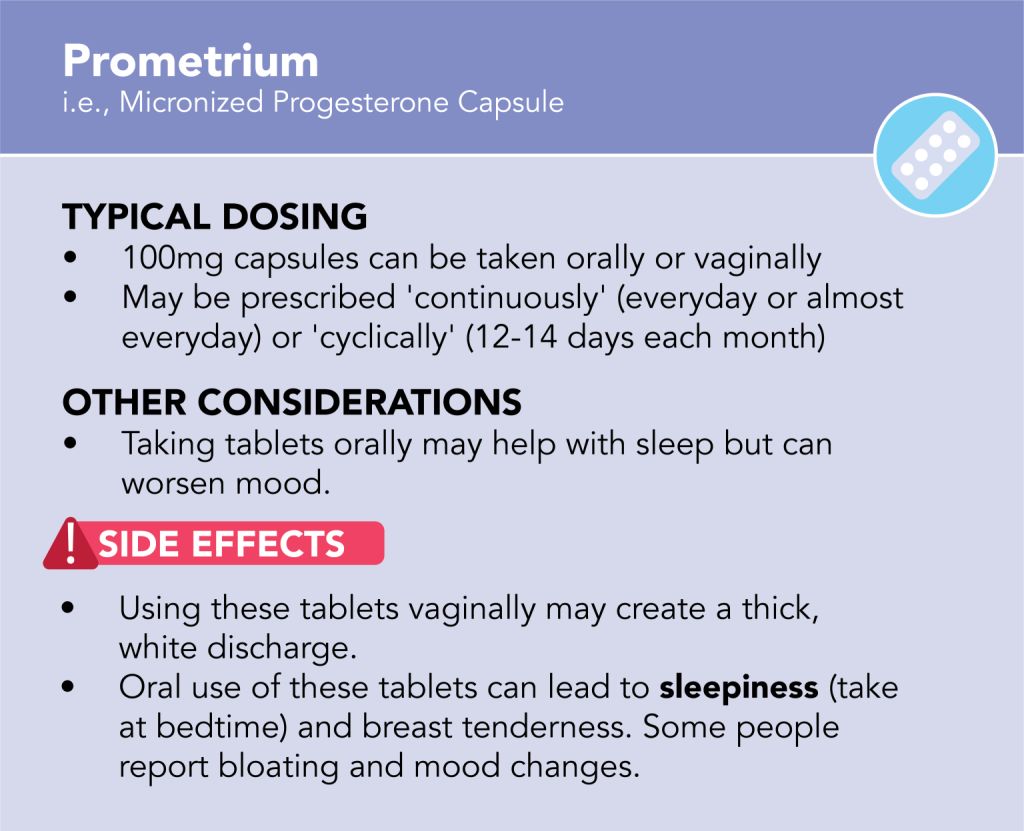
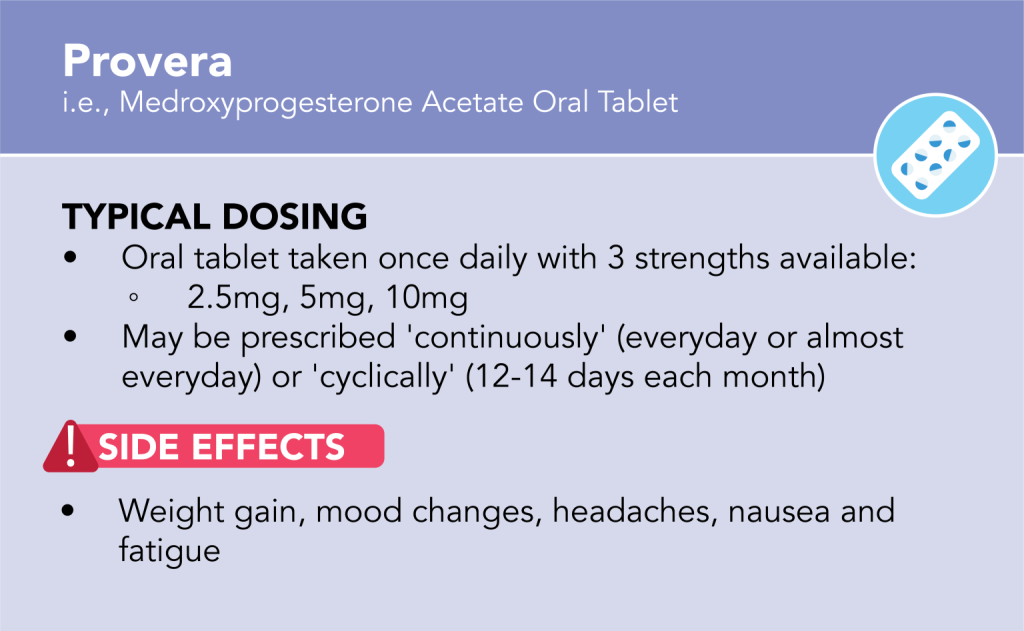
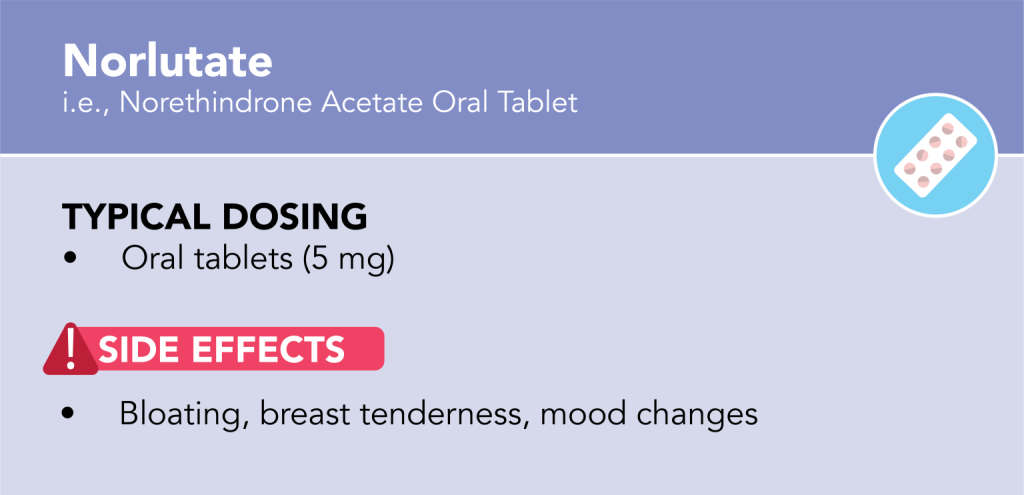
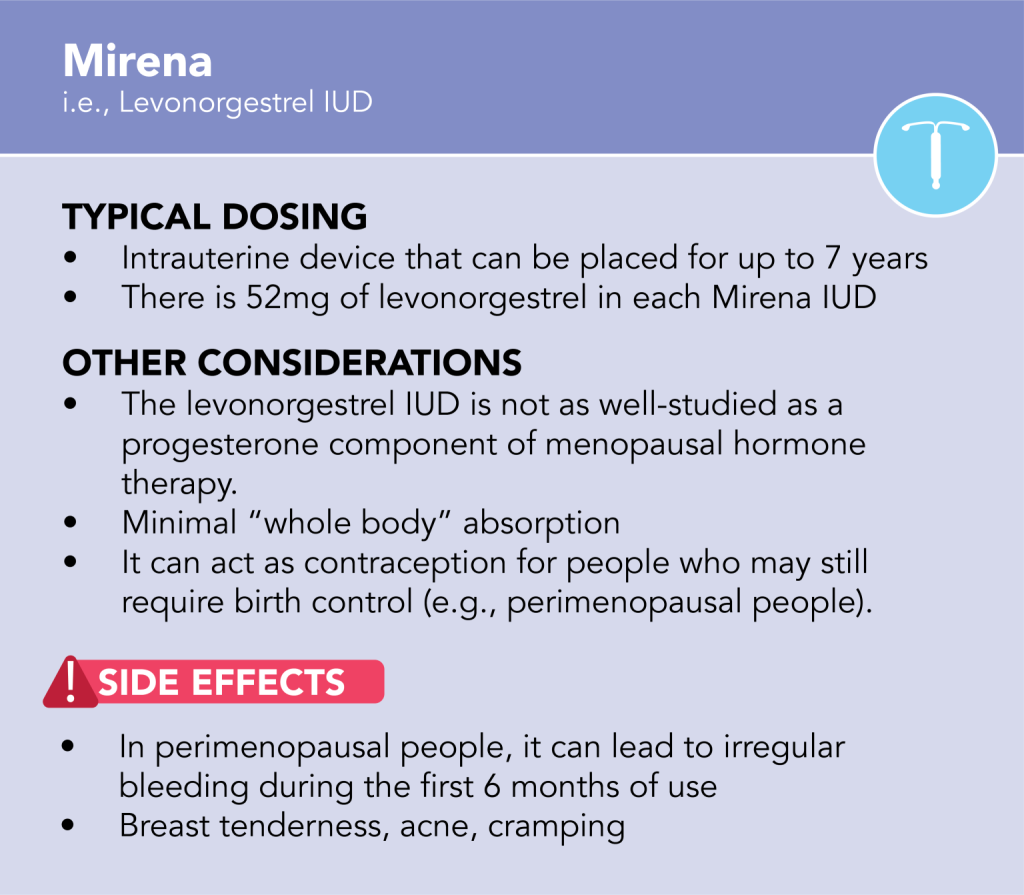
Progesterone can be given through an intrauterine device (e.g., Mirena IUD) or tablets (oral or vaginal administration). Tablets can be prescribed cyclically (12-14 days per month) or continuously (everyday or almost everyday).
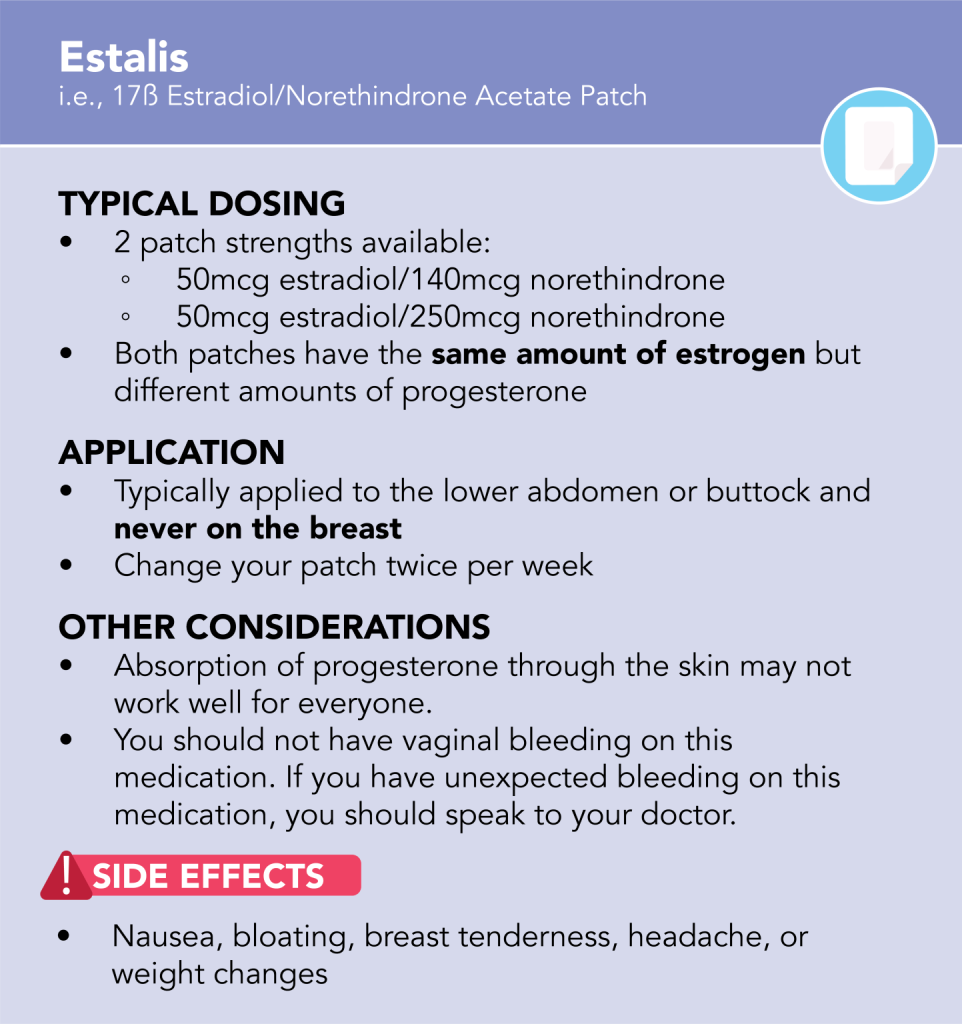
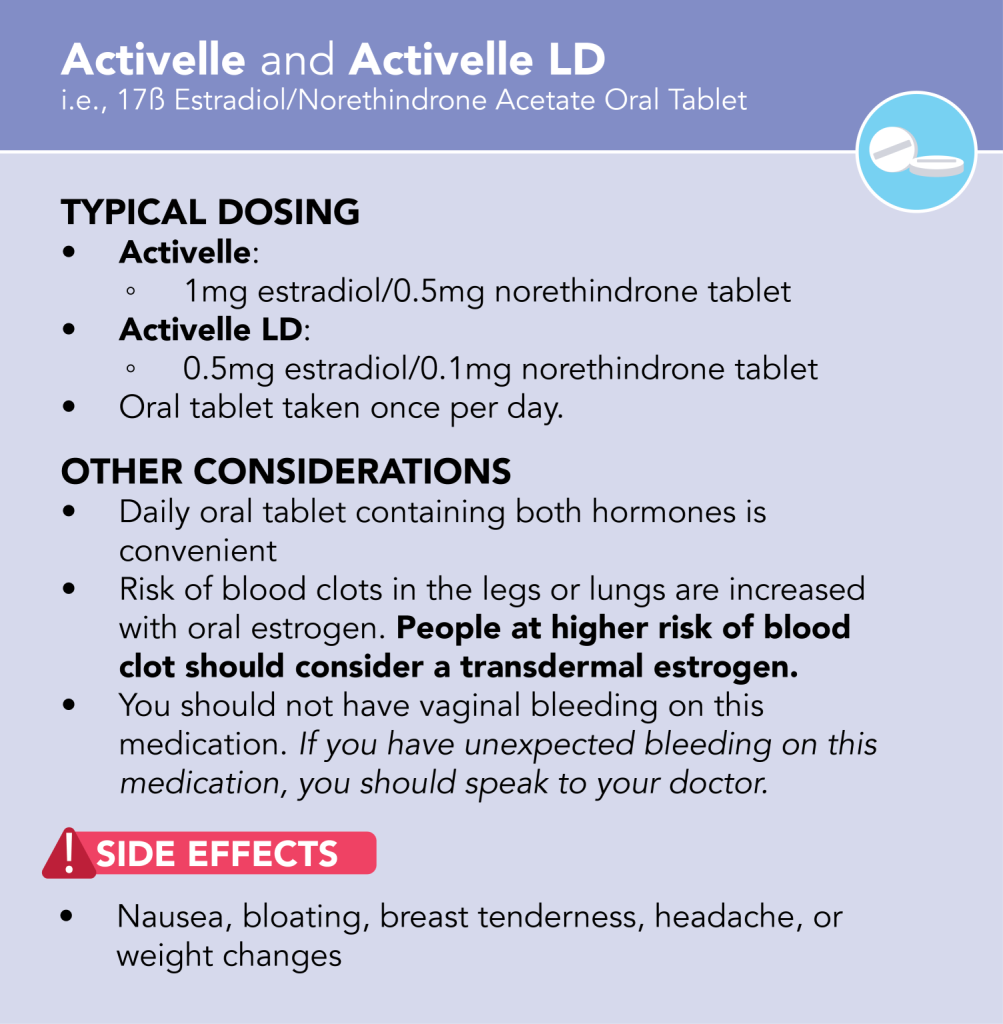
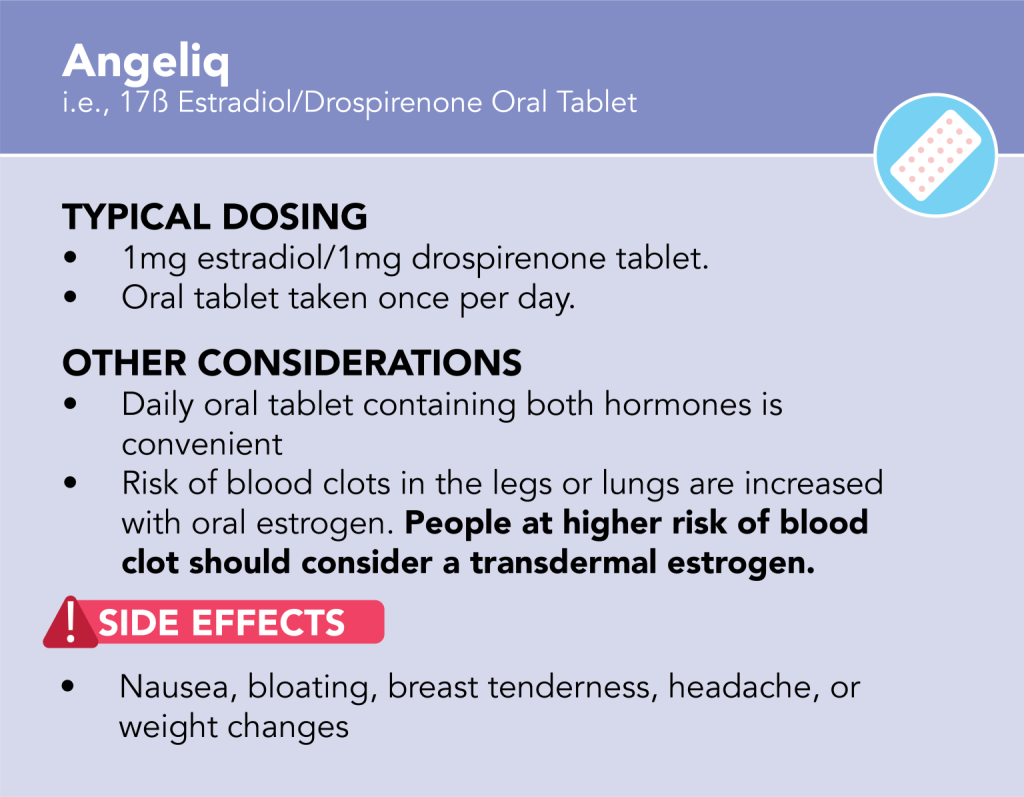
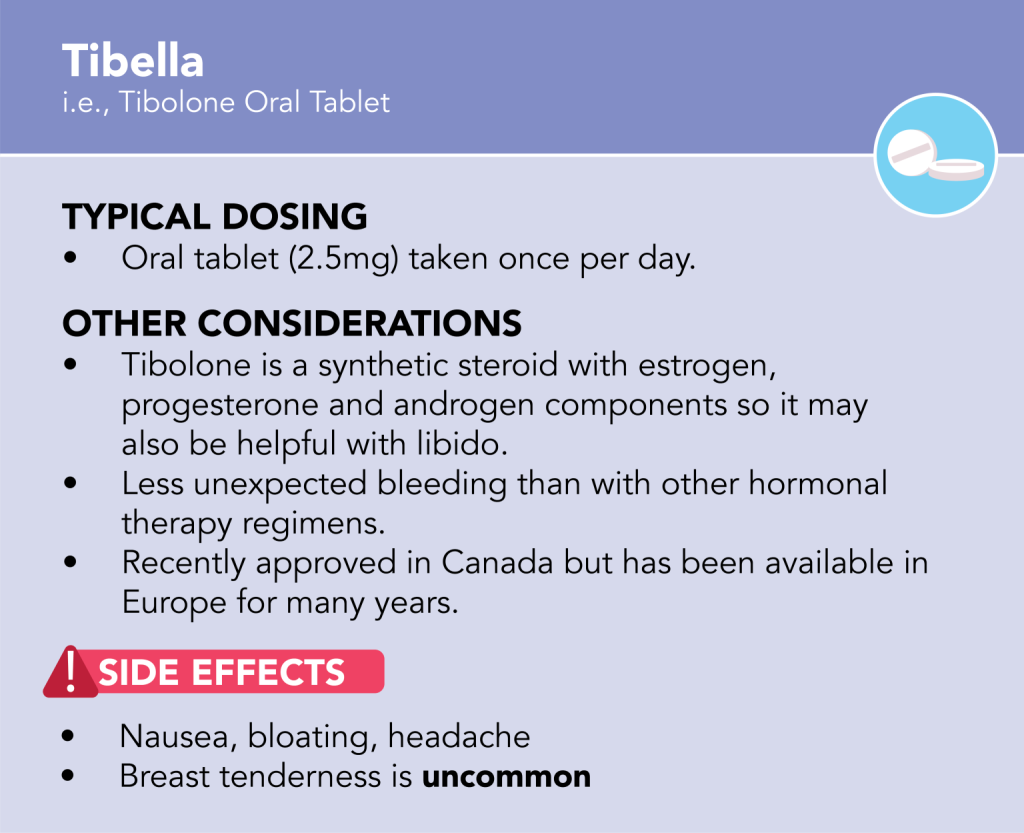
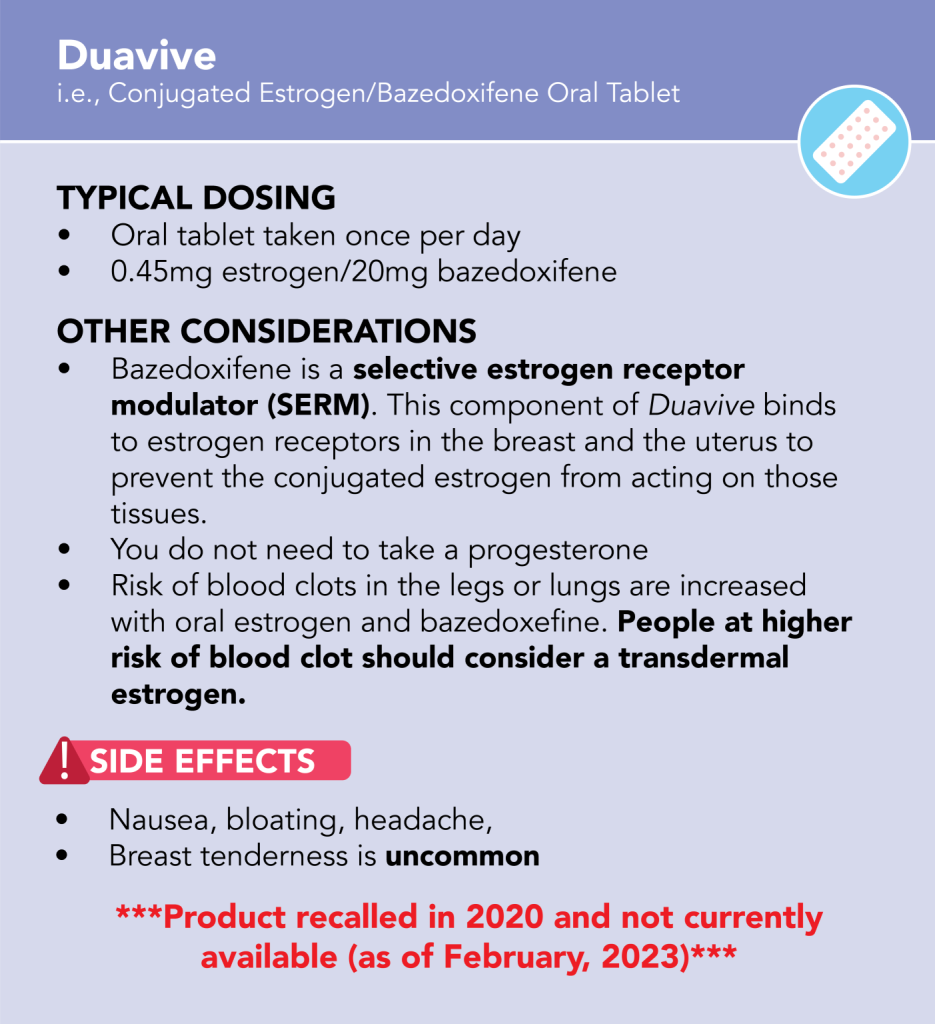
Combination Estrogen & Progesterone

Some systemic hormone therapy products are ‘Combination’ products. This eliminates the need to take a second medication in
people with a uterus.
Video Resources
Common Systemic Hormone Therapy Products(Available in Canada)
Estrogen/Progesterone
Combination Products
Handouts
Some people should not use these medications.
Click HERE to find out more.
Systemic Hormones Therapy FAQs
Your doctor will individualize your dose based on your symptoms, age and risk profile. Younger women typically require higher estrogen doses for bone and cardiovascular protection.
Higher doses of estrogen require higher doses of progesterone for endometrial protection. There can be more side effects and risks with higher doses of systemic hormone therapy.
You will experience the maximum effect of your MHT after 12 weeks, but for those with very severe symptoms, you may experience some relief within the first week of use. Doctors tend to review and make adjustments to hormone therapy regimens 12 weeks after starting.
When lowering your dose of hormone therapy, you likely will not feel the full impact of the decrease until 8 weeks later.
The best time to start MHT is before age 60 and less than 10 years since a final menstrual period but there is no universal right time to stop.
Risk of heart attack, stroke and blood clot increase in people older than 60 years and/or more than 10 years from their final menstrual period.
However, age is never the only reason to stop systemic MHT and shared decision-making should happen between you and your doctor.
Menopause hormone therapy helps to mask menopausal symptoms but doesn’t change what your body is meant to do. Treatment should be individualized and each person should be on the lowest effective dose to control their symptoms for the shortest amount of time.
By slowly lowering your dose of MHT (weaning), you will learn more information about the minimum effective dose for you. By going slowly, you can also minimize interference with your quality of life. It is less advisable to completely discontinue and then restart MHT for extended periods of time, as your highest risk of a blood clot is in the first 3-6months of use.
In any form, estrogen slightly increases the risk of blood clot. Estrogen through the skin (transdermally) may decrease your risk compared to oral tablets.
When taken together, estrogen and progesterone can increase risk of breast cancer by 1 extra case per 1000 women per year for the average person.
In healthy people, risks increase after the age of 60 or when someone is more than 10 years from a final menstrual period.
Speak to your doctor for a personalized discussion about risks of systemic menopausal hormone therapy that apply to you.