Menopause Symptoms & Treatments
Each person’s experience with menopause is different. Many people who have natural menopause will report no symptoms except for irregular periods that eventually stop when they reach menopause. While you may experience symptoms that aren’t described here, the most common symptoms of menopause and treatment options are explained below.
Common Menopausal Symptoms
Click on each image to learn more.
Vasomotor Symptoms
(Hot Flashes & Night Sweats)
VMS include hot flashes and night sweats, often described as sudden wave-like sensations of heat. They can be accompanied by anxiety or palpitations.
The cause of vasomotor symptoms is not well understood but has to do with estrogen’s effect on the body’s ability to regulate temperature.

Treating Vasomotor Symptoms
There are different treatments available for hot flashes and night sweats (vasomotor symptoms). These can be divided into several broad categories:
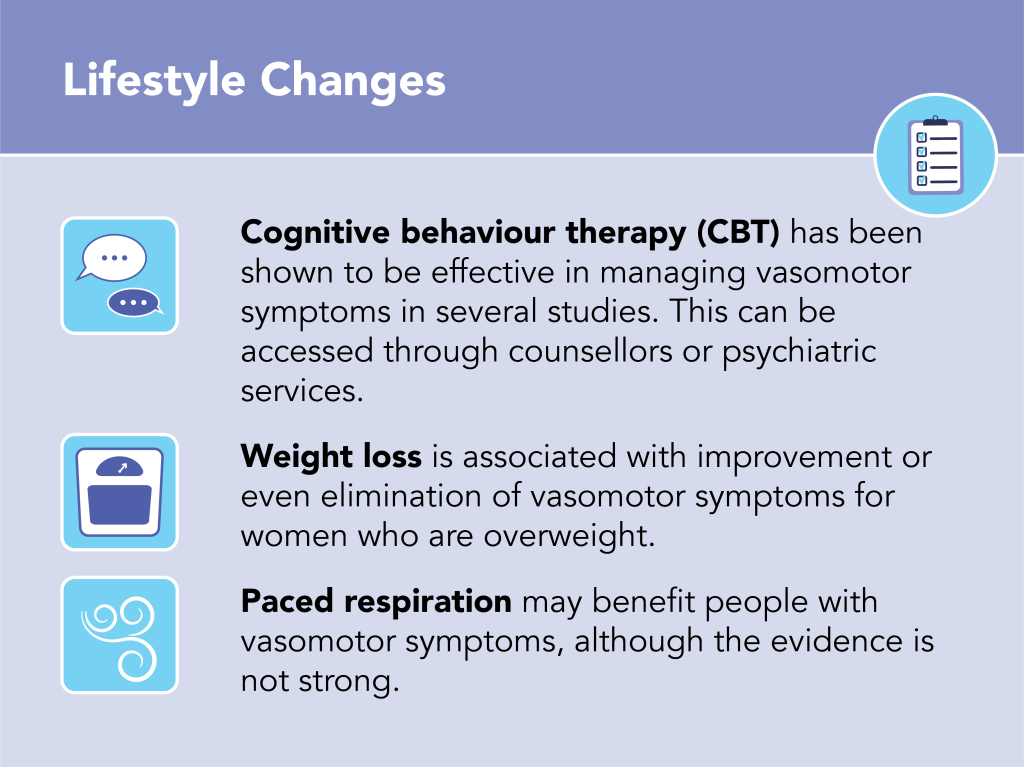
- Lifestyle Changes
- Naturopathic and Complementary Medicines
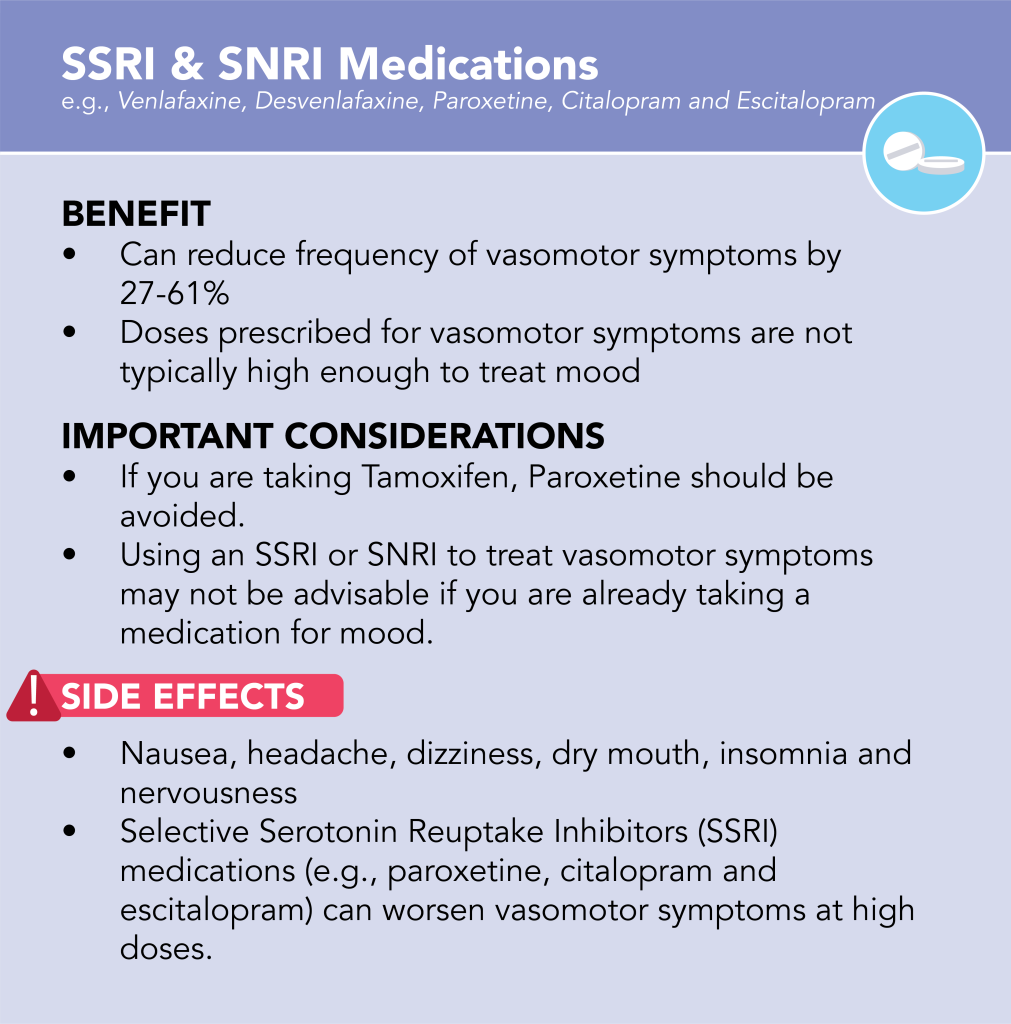
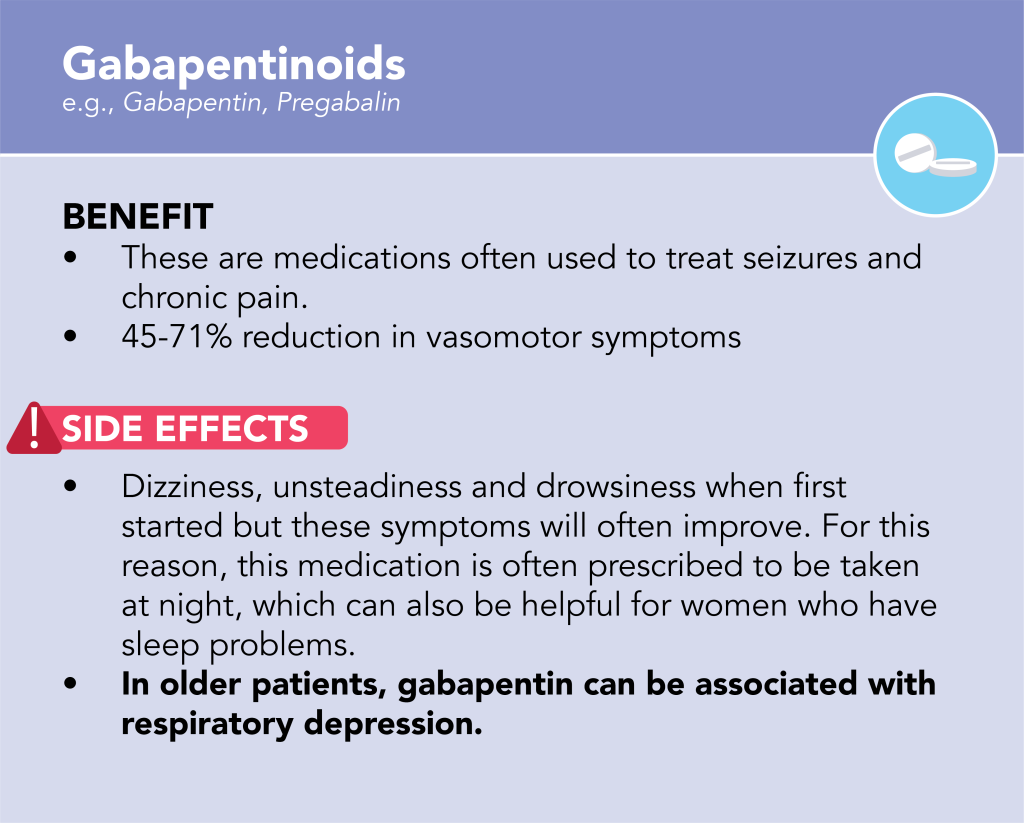
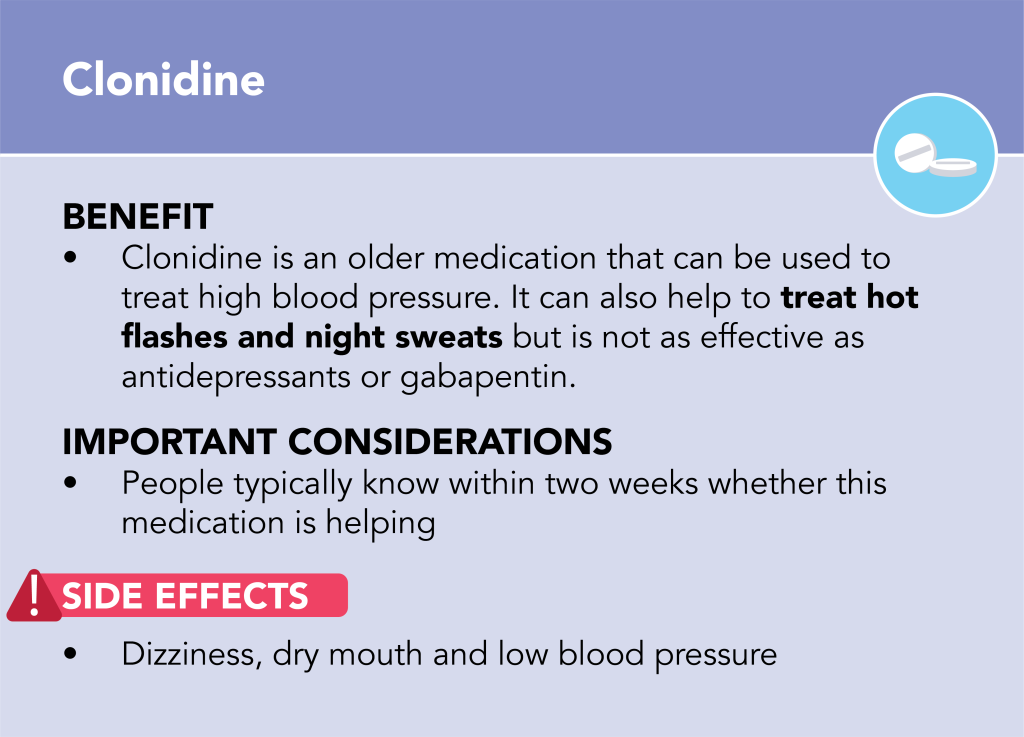
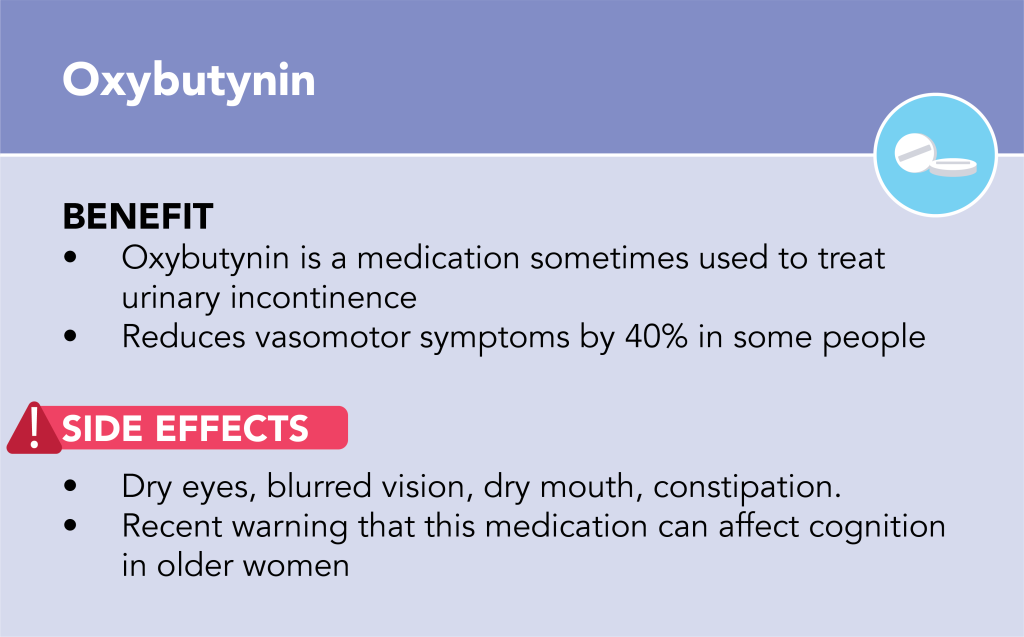
- Non-Hormonal Prescription Medications
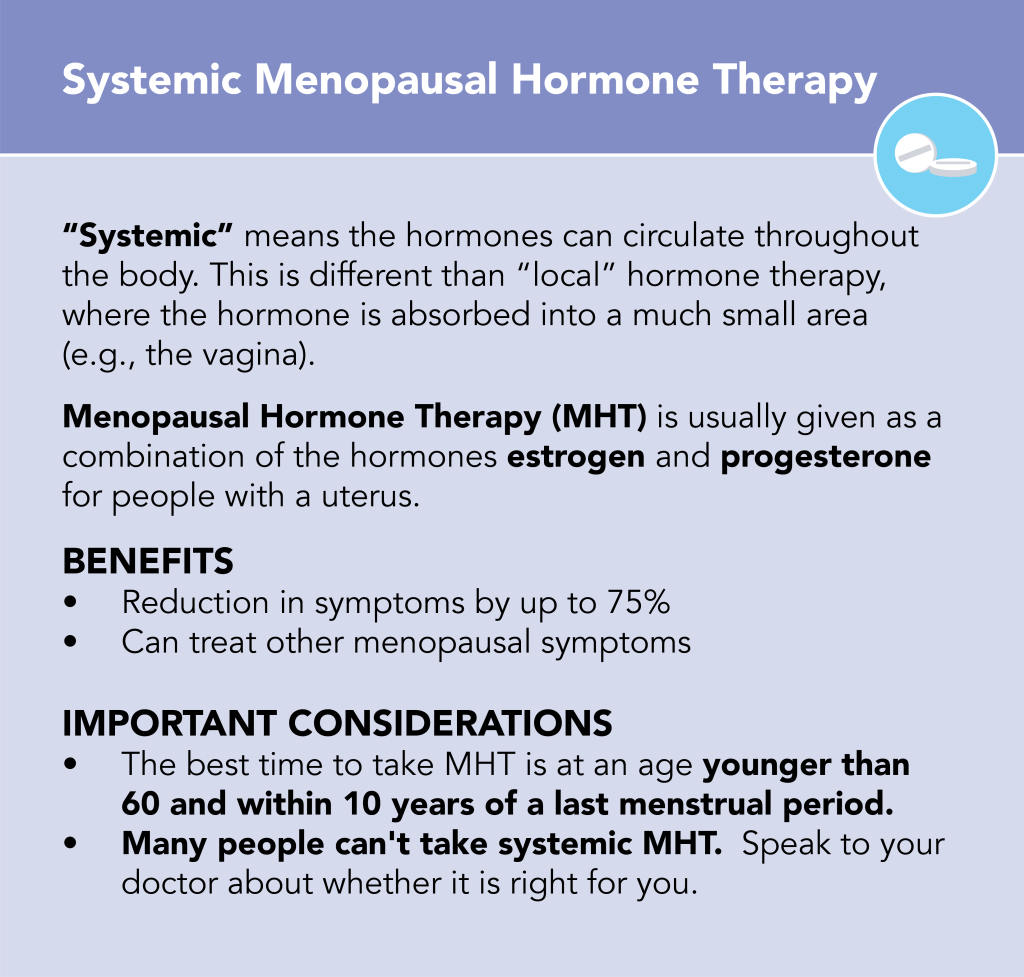
- Menopausal Hormone Therapy (MHT)
Your treatment should be personalized and based on your symptoms, personal preferences and past medical and family history. Speak to your doctor about treatments that are best for you.
Video Resources
Fast Facts
Handouts
Genitourinary Syndrome of Menopause




GSM can cause changes in the outward appearance of the vulva, including shrinking of the labia minora, loss of pubic hair, narrowing of the opening of the vagina, changes in vaginal discharge and paler colour of the skin.
GSM occurs in about 40-50% of menopausal people.

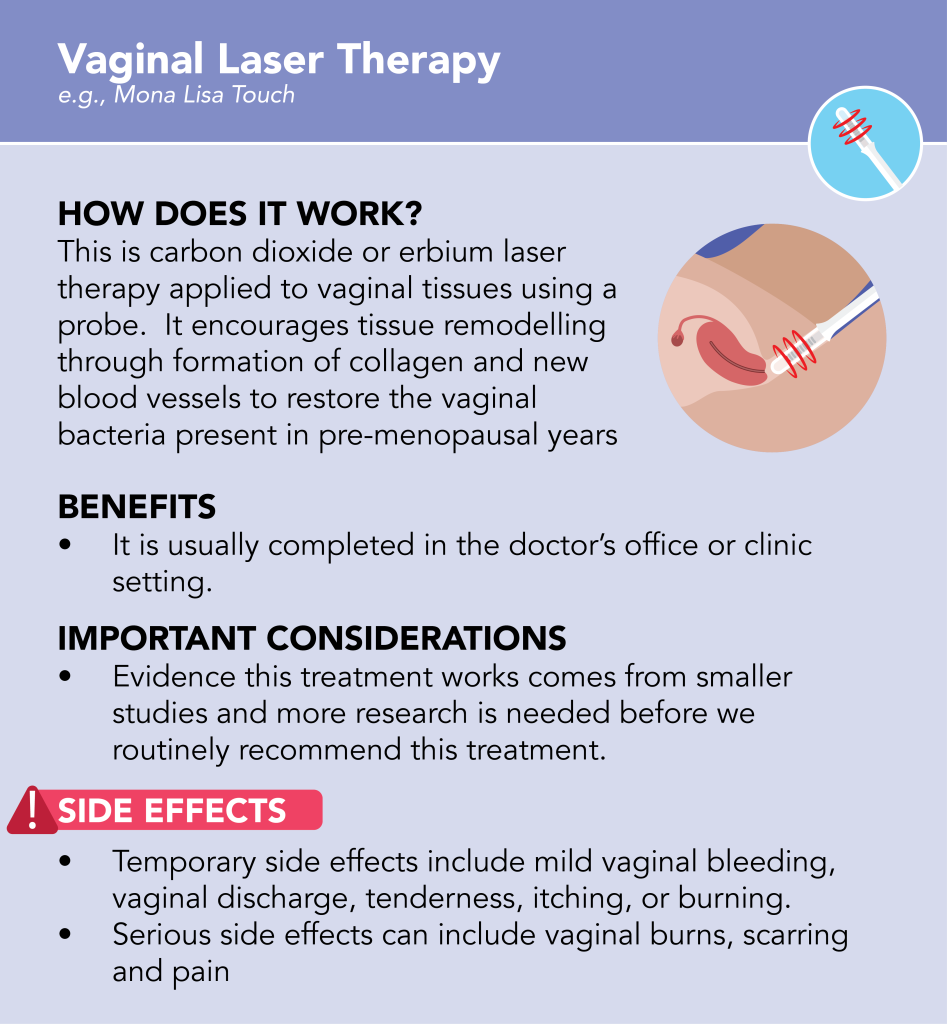
Treating Genitourinary Syndrome of Menopause
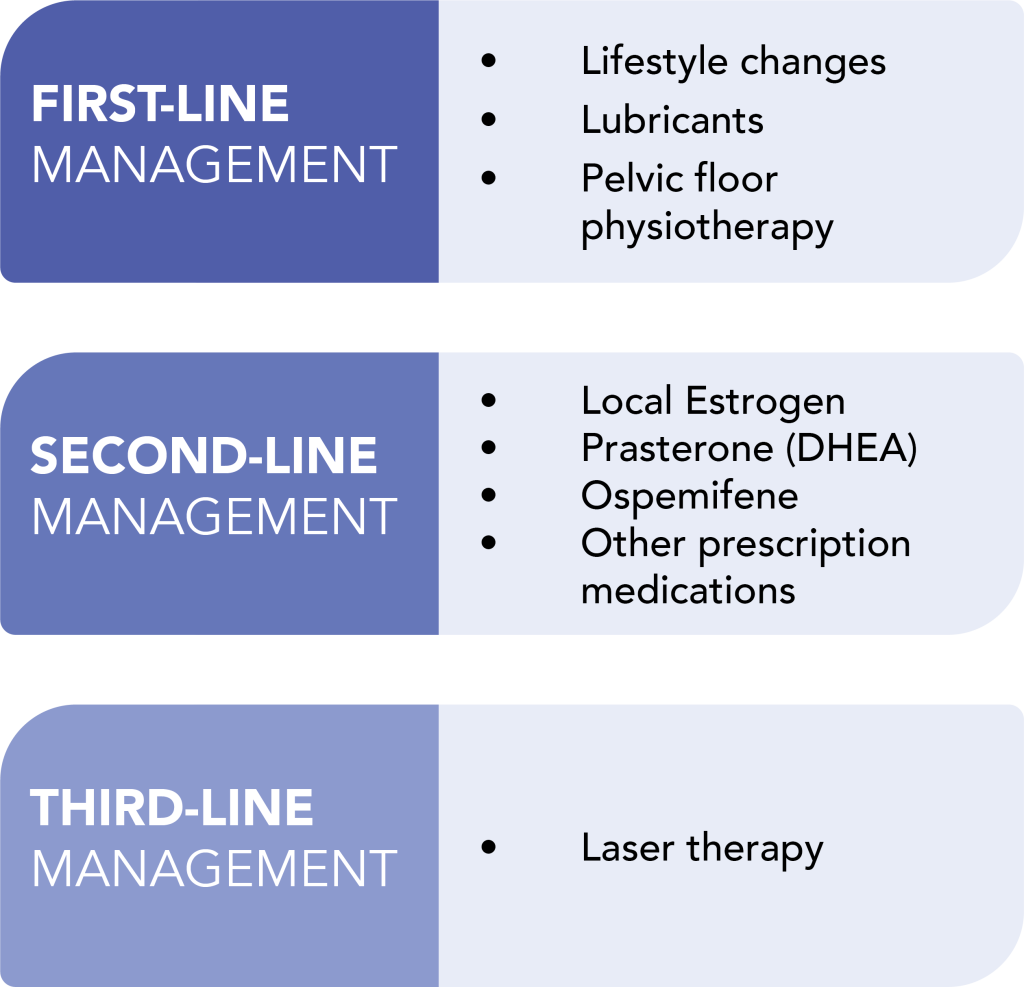
There are different treatments available for genitourinary symptoms. These can be divided into first-, second- and third-line treatment categories.
What you choose will be based on your symptoms, personal preferences and past medical history.
Navigating through the resources below will help you learn more about different treatments for genitourinary symptoms. Speak to your doctor about treatments that are best for you.
Video Resources
Fast Facts
Handouts
Sexual Concerns
The most common sexual concerns associated with menopause are loss of libido (sex drive) and pain with sex (dyspareunia)
Many factors can affect sex drive, including menopause. Other factors include stress, body image, past sexual experiences, partner factors, medication and drugs, and other personal health/medical issues. In addition, the vulva and vaginal changes associated with the genitourinary syndrome of menopause (GSM) can affect desire, and cause discomfort or pain with sex. This can affect arousal and orgasm.
Up to 50% of people report low sex drive. Sexual problems can be more common in people who undergo surgical menopause, or who undergo early menopause (before the age of 45).
Sexual function is multifactorial, and there is no normal. Any sexual issue that causes you distress is worth speaking to your health care provider about.

Addressing Sexual Concerns
Sexual function and libido are multifactorial. This means lots of factors can have an impact. Proper treatment of sexual concerns starts with education about the effects of aging, health concerns and medications. Begin optimizing your sexual health by considering:
- Treatment of Genitourinary Syndrome of Menopause if this is something you have. Learn more about this here.
- Strategies to improve relationships
- Optimizing treatments for other health conditions, such as anxiety, depression, urinary incontinence and thyroid concerns
Pain with Sex (i.e., dyspareunia) can be helped with lubricants, vaginal moisturizers and local hormone therapy, as well as pelvic floor physiotherapy. A link to our patient handout on Dyspareunia can be found here.
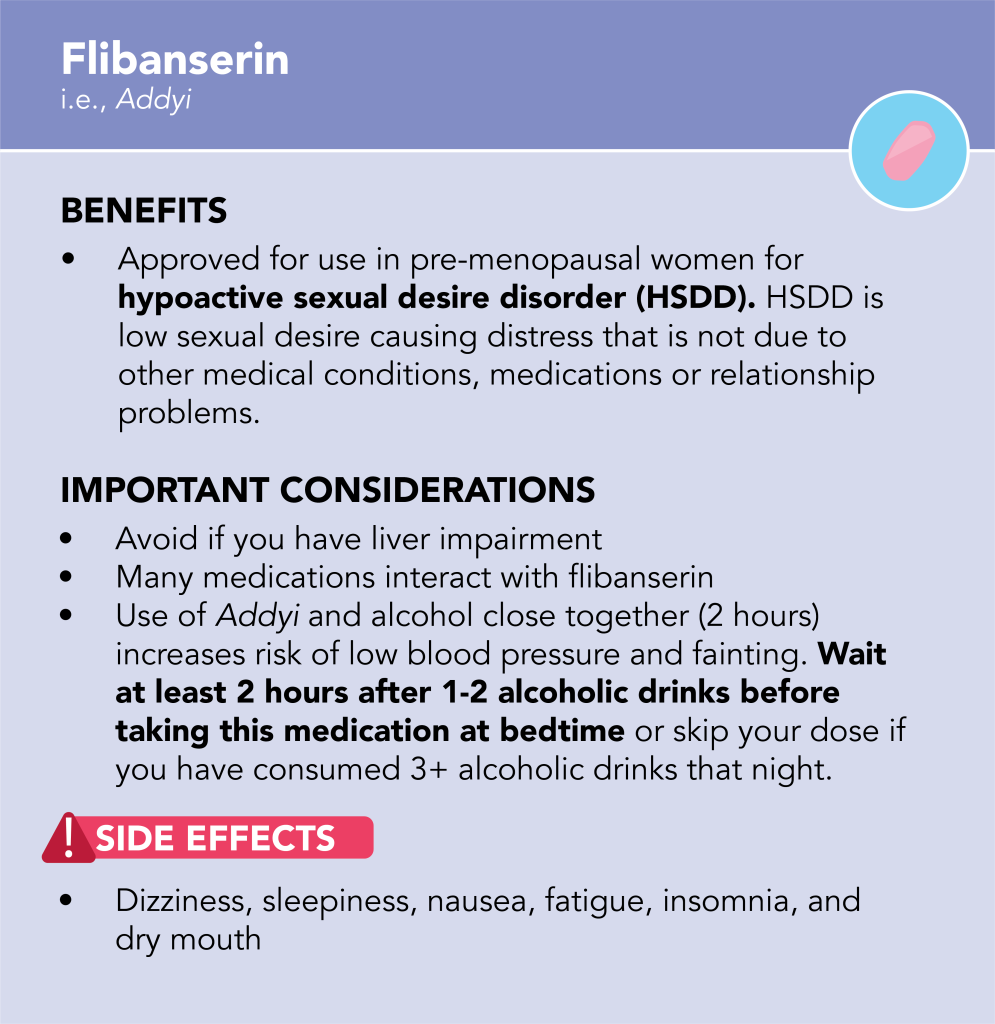
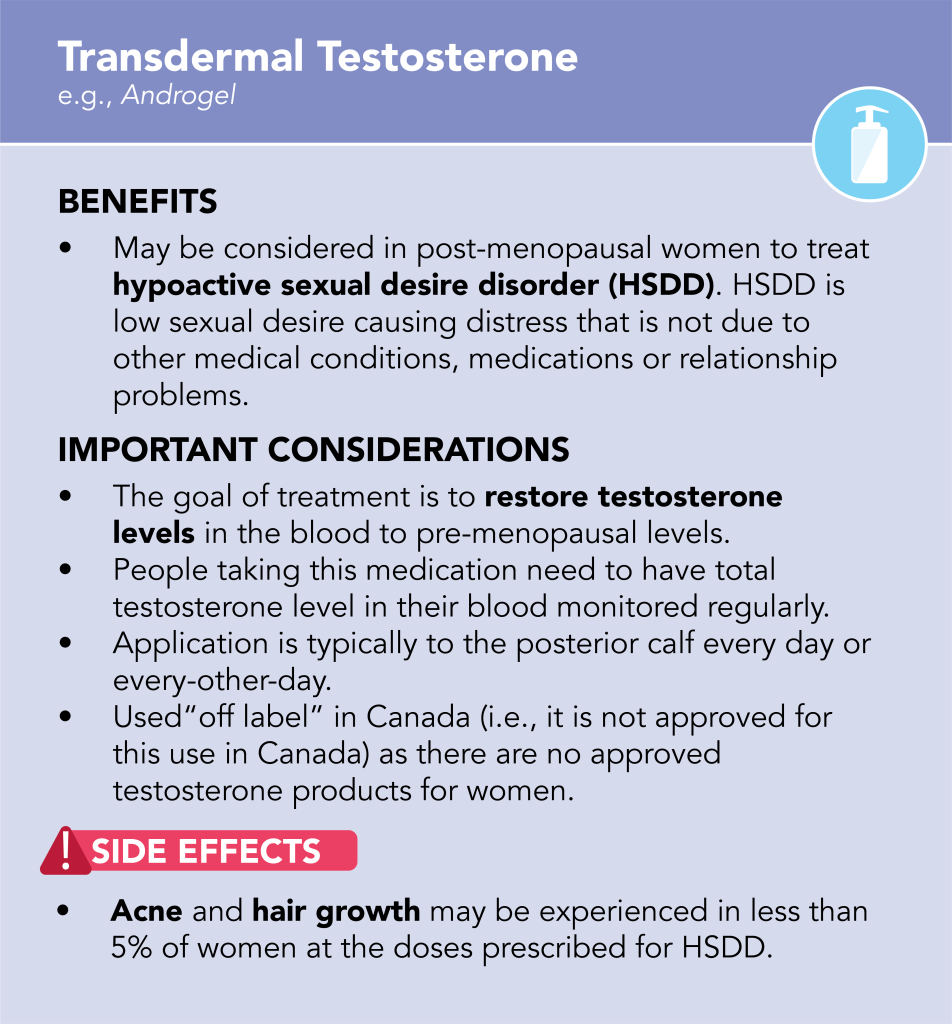
Low sex drive can sometimes be treated with transdermal testosterone therapy. In Canada, using testosterone gel for this reason is considered “off label” use. In pre-menopausal women, Flibanserin (Brand Name: Addyi) can also be considered. These medications can have side effects and require careful monitoring. Speak to your doctor about whether they could be considered for you.
Fast Facts
Handouts
Mood Changes
Depressive symptoms can increase in the menopausal transition. People who have a history of depression, major depressive episodes, premenstrual syndrome (PMS) and postpartum depression may be at higher risk of having these symptoms occur.
The menopausal transition can also be a time where people are at risk of developing anxiety, either new-onset, or recurrent. This can also be associated with the frequency and intensity of vasomotor symptoms, such as hot flashes and night sweats.
Mood changes have been observed in up to 25% of people.
Treating Mood Changes
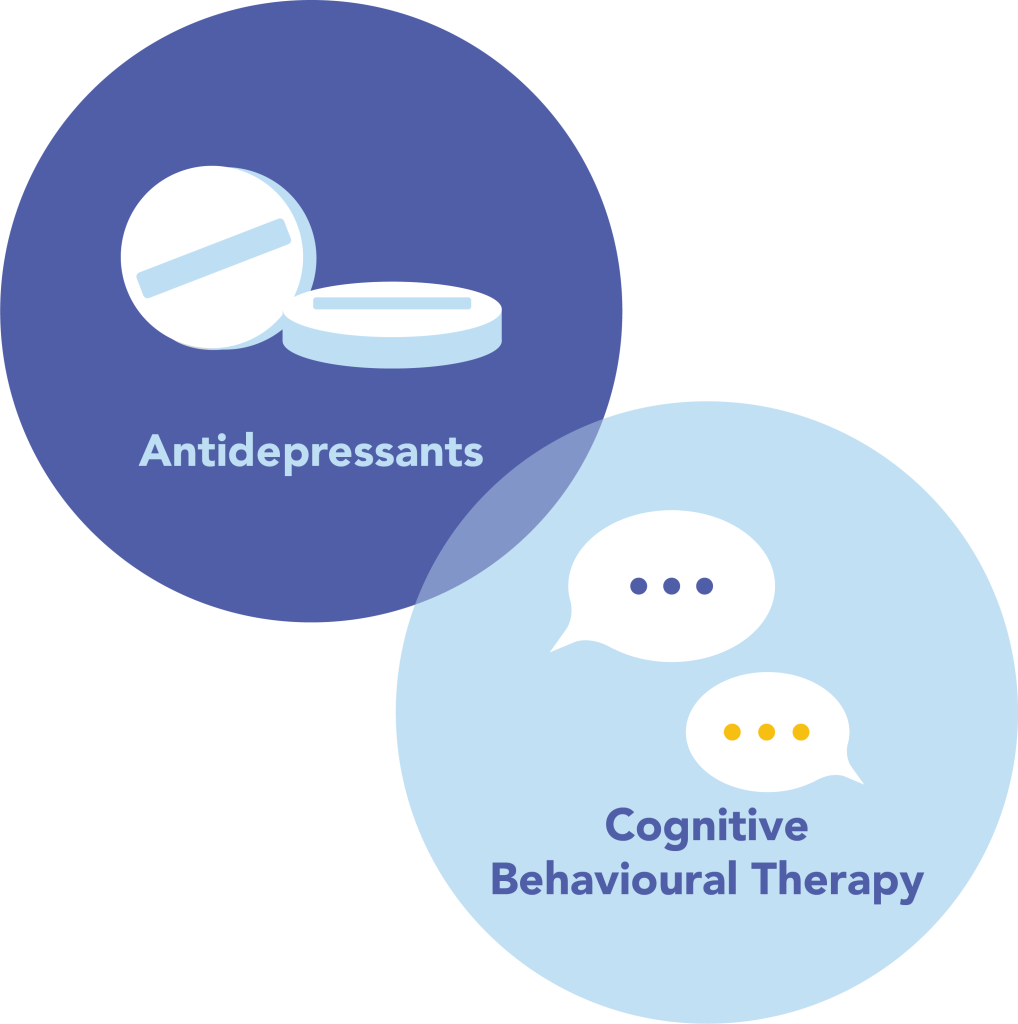
Antidepressants and Cognitive Behavioural Therapy (CBT) are first-line treatments for depressive disorders and depressive symptoms for menopausal women.
It is important to determine whether mood changes started at the time of menopause, or are pre-existing. For women who are already taking an antidepressant medication, some dose changes may be required around the time of menopause to improve mood.
Some people will have mood benefits from Menopausal Hormone Therapy (MHT), especially women in perimenopause. For those experiencing both vasomotor symptoms and mood symptoms, MHT can be helpful.
There is also evidence for regular exercise and mindfulness-based therapies to improve mood.
Cognitive Changes
Many people will report forgetfulness and difficulty with concentration during the menopausal transition, which is sometimes referred to as “brain fog”. This can worsen in the first year after the last menstrual period. Vasomotor symptoms, depression, and anxiety can also have an effect on cognitive function.

Addressing Cognitive Changes
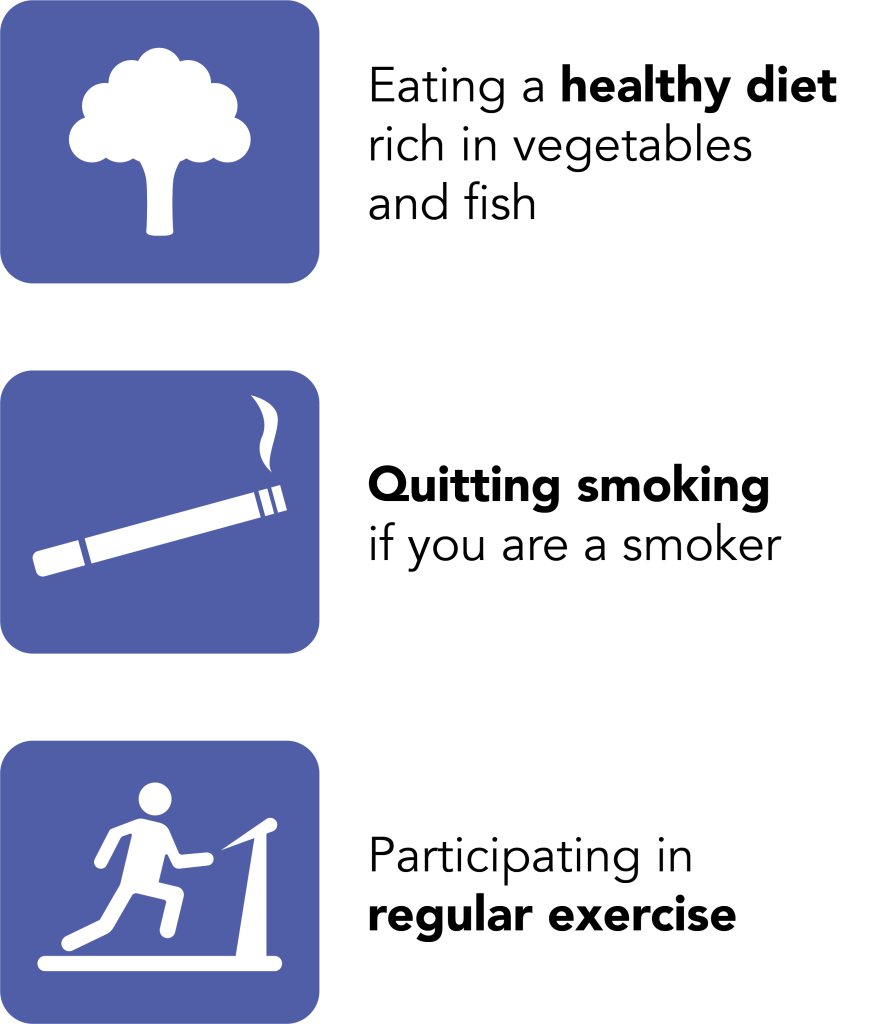
Aging can impact cognition. Cognitive function can be optimized through diet, exercise and quitting smoking.
Sometimes, treating hot flashes, night sweats and mood symptoms can help to improve brain function. If you are concerned about your cognition, speak to your doctor. Many conditions, other than menopause, can affect cognition. It is important for you to discuss your personal symptoms with a healthcare provider.
Sleep Concerns
Disrupted sleep and poor sleep quality are common issues for many people in the menopausal transition. Vasomotor symptoms (hot flashes and night sweats) can cause significant sleep disturbance. Sleep can also be affected stress, sleep apnea, restless leg syndrome, overactive bladder, certain medications and a history of difficulty with sleep.
Disrupted sleep affects about 30% of menopausal people.

Addressing Sleep Concerns
Sleep hygiene is an important part of managing sleep disturbances. Sleep hygiene can include:
- Maintaining the same bedtime and wake up time
- Using bedroom only for sleep and intimate encounters
- Limiting electronics before bedtime
- Avoiding alcohol and caffeine
Cognitive Behavioural Therapy (CBT) has also been shown to help to treat insomnia.
Addressing sleep concerns due to health conditions such as sleep apnea, restless leg syndrome and overactive bladder is also important.

Generate a PersonalizedMenopause Education Package
Coming Soon!