Table of Contents
- Summary
- Diagnosing Endometrial Polyps
- Transvaginal Ultrasound
- Sonohysterogram
- Tissue Biopsy
- Diagnosing and Treating Polyps for Better Health
Summary:
- Diagnosing endometrial polyps often starts with imaging, like a pelvic and/or transvaginal ultrasound, to explore symptoms such as abnormal bleeding. Polyps cannot be diagnosed through blood work.
- In some cases, a sonohysterogram provides a more detailed view of the uterine cavity for clearer assessment.
- If there are cancer risk factors, an endometrial biopsy may be performed to sample the uterine lining.
- For precise diagnosis and removal, a hysteroscopic polypectomy may be recommended, allowing targeted excision under direct visualization.
Diagnosing endometrial polyps typically begins with imaging, such as a pelvic and/or transvaginal ultrasound, to investigate symptoms like abnormal bleeding. In some cases, a sonohysterogram is used for a more detailed view of the uterine cavity. If cancer risk factors are present, an endometrial biopsy or a hysteroscopic polypectomy may be recommended for precise diagnosis and removal.
These steps allow physicians to tailor a treatment plan that addresses each patient’s specific health needs.
Diagnosing Endometrial Polyps
Endometrial polyps cannot be diagnosed through blood work and typically require imaging as the first step. They are often identified during evaluations for other symptoms or concerns, such as abnormal vaginal bleeding or infertility.
Transvaginal Ultrasound
For suspected endometrial polyps, your physician will typically begin with a pelvic and/or transvaginal ultrasound (TVUS) as the initial imaging approach.
- A pelvic ultrasound uses an external probe on your lower abdomen to capture images of your pelvic structures.
- With your consent, a transvaginal ultrasound may also be performed at the same time. During a TVUS, a probe is gently inserted into the vagina to provide clearer images of the reproductive organs.
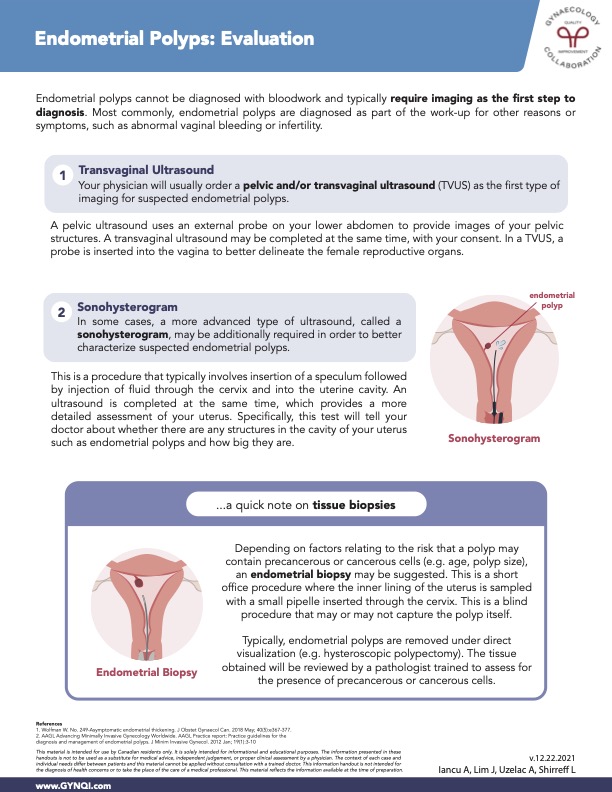
Sonohysterogram
In some cases, a more advanced ultrasound, known as a sonohysterogram, may be needed for a clearer evaluation of suspected endometrial polyps. This procedure typically involves inserting a speculum, followed by gently injecting fluid through the cervix into the uterine cavity.
An ultrasound is then performed, allowing for a more detailed view of the uterus. This provides information on the presence and size of any structures, such as endometrial polyps, within the uterine cavity.
Tissue Biopsy
Based on factors such as age and polyp size, which can influence the risk of precancerous or cancerous cells, an endometrial biopsy may be recommended. This quick office procedure involves sampling the uterine lining with a small pipelle inserted through the cervix. Because it is a blind procedure, it may or may not capture the polyp itself.
For more precise removal, polyps are typically excised under direct visualization through a hysteroscopic polypectomy. The collected tissue is then reviewed by a pathologist to check for any precancerous or cancerous cells.
Diagnosing and Treating Polyps for Better Health
Diagnosing and managing endometrial polyps often requires a series of imaging and, when needed, tissue sampling procedures. Pelvic and/or transvaginal ultrasounds, provide a clear view of the pelvic structures. For a more detailed assessment, a sonohysterogram may be used to better visualize the uterine cavity.
In cases where cancer risk is a concern, an endometrial biopsy or hysteroscopic polypectomy may be recommended to examine tissue samples for precancerous or cancerous cells.
Together, these diagnostic tools ensure a thorough evaluation to guide appropriate treatment and care.



