Table of Contents
- Summary
- What is Hysteroscopy?
- How is a Hysteroscopy Performed?
- Different Types of Hysteroscopy
- Diagnostic Hysteroscopy
- Operative Hysteroscopy
- Risks of Hysteroscopy
- Recovery from Hysteroscopy
- Empowering Yourself in Your Health Journey
Summary:
- Hysteroscopy uses a camera-equipped instrument to examine the inside of the uterus through the vagina and cervix.
- Most procedures are done under general anesthesia, but some can be completed while the patient is awake in a clinical setting.
- Hysteroscopy allows the doctor to visualize abnormalities, take biopsies, or remove uterine tissues like polyps and fibroids.
- Patients usually experience minimal recovery time with mild cramping and light bleeding, typically resuming normal activities the same day.
Hysteroscopy is a minimally invasive procedure that allows your doctor to examine the inside of your uterus using a slender, camera-equipped instrument called a hysteroscope. The hysteroscope is inserted through the vagina and cervix into the uterus, providing a clear view of the uterine cavity. Most hysteroscopies are performed under general anesthesia, though some can be done while the patient is awake in a clinical setting. This procedure can be used for both diagnostic and operative purposes, helping to evaluate or treat various conditions within the uterus with minimal recovery time.
What is Hysteroscopy?
Hysteroscopy is a minimally invasive procedure that allows your doctor to see inside the uterus. A hysteroscope is a slender telescope instrument with a camera and light attached. It is inserted through the vagina, past the cervix, and into the uterus.
Most hysteroscopies are done while patients are asleep. However, some procedures can be offered while patients are awake and are done in a clinic setting.
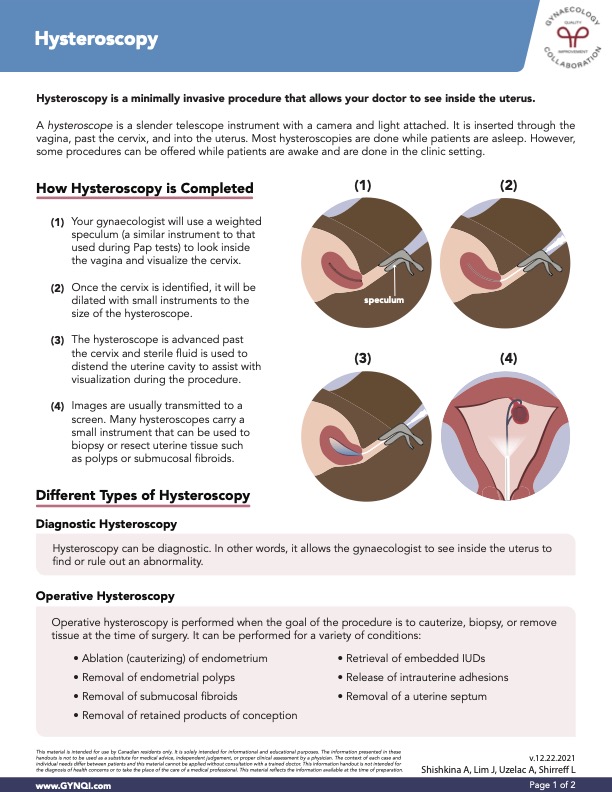
How is a Hysteroscopy Performed?
Below is a step-by-step guide to how a hysteroscopy is generally performed.
Step One: Your gynecologist will use a weighted speculum, similar to the instrument used during Pap tests, to examine the vagina and visualize the cervix.
Step Two: Once the cervix is identified, it will be dilated with small instruments to the size of the hysteroscope.
Step Three: The hysteroscope is advanced past the cervix and sterile fluid is used to distend the uterine cavity to assist with visualization during the procedure.
Step Four: Images are usually transmitted to a screen. Many hysteroscopes carry a small instrument that can be used to biopsy or resect uterine tissue such as polyps or submucosal fibroids.
Different Types of Hysteroscopy
There are two main types of hysteroscopy—diagnostic and operative—each serving distinct purposes in evaluating and treating conditions within the uterus.
Diagnostic Hysteroscopy
A hysteroscopy can be performed for diagnostic purposes. In other words, it allows the gynaecologist to see inside the uterus to find or rule out an abnormality.
Operative Hysteroscopy
Operative hysteroscopy is performed when the goal of the procedure is to cauterize, biopsy, or remove tissue at the time of surgery. It can be performed for a variety of conditions:
- Ablation (cauterizing) of endometrium
- Removal of endometrial polyps
- Removal of submucosal fibroids
- Removal of retained products of conception
- Retrieval of embedded IUDs
- Release of intrauterine adhesions
- Removal of a uterine septum
Risks of Hysteroscopy
Although hysteroscopy is generally a safe procedure, it does carry some risks. These can include:
Bleeding: This most commonly happens because of bleeding from the surgical site, but can be due to a cut on the cervix or from uterine perforation. Depending on the location and cause of the bleeding, your surgeon will use different methods to stop it.
Infection: This occurs in under 1% of cases and is usually managed with antibiotics.
Excess Fluid Absorption: This can occur when too much sterile fluid, that is used to distend the uterus, is absorbed by the body. It can cause low sodium levels in the blood. The effects are usually mild but at times can require treatment and/or hospital stay to correct the sodium levels.
Injury to the Cervix: A cut on the cervix (laceration) can occur during any part of the procedure. If this occurs, the surgeon will repair the cervix with stitches.
Uterine Perforation: An inadvertent injury to the muscular wall of the uterus can create a small hole. In this case, the hysteroscope passes through the uterine wall into the abdominal cavity. It occurs in 0.1% of diagnostic hysteroscopy cases and 1% of operative hysteroscopies. Some patients may be at higher risk.
Damage to Surrounding Structures: A uterine perforation may result in injury to the bowel, bladder, and blood vessels. These injuries may require a laparoscopy or a larger incision on the abdomen to explore and repair any injury to these structures.
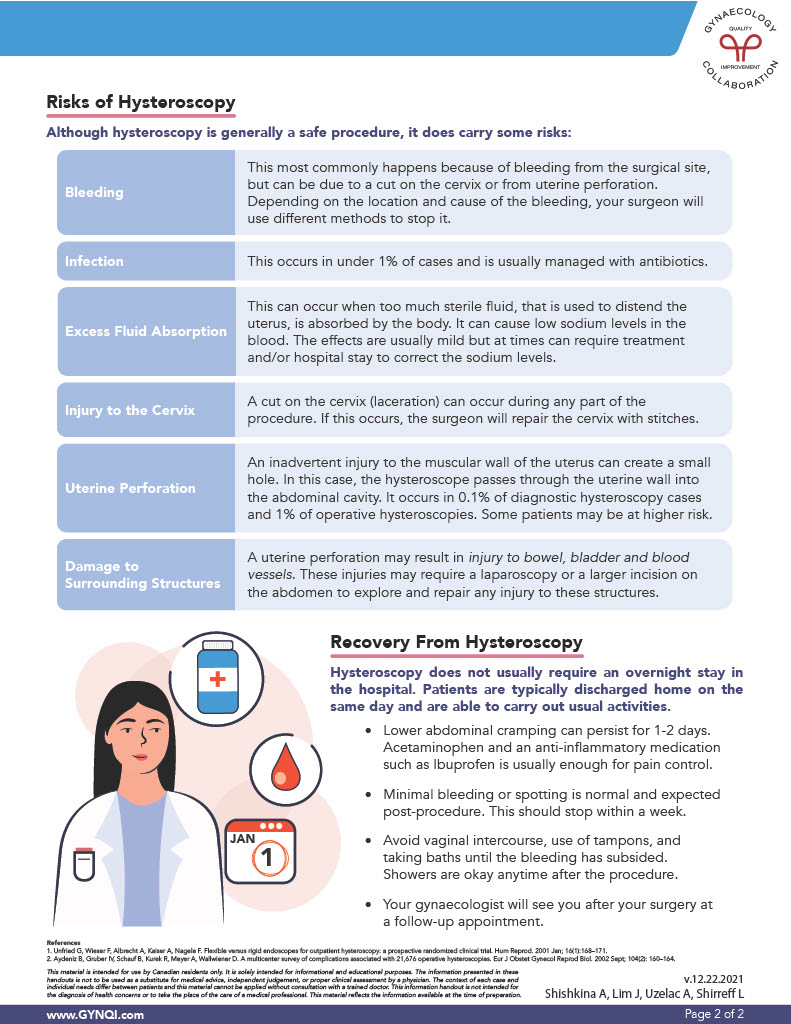
Recovery From Hysteroscopy
Hysteroscopy does not usually require an overnight stay in the hospital. Patients are typically discharged home on the same day and are able to carry out usual activities.
Post-surgery care can include:
- Lower abdominal cramping that can persist for 1-2 days. Acetaminophen and an anti-inflammatory medication such as Ibuprofen are usually enough for pain control.
- Minimal bleeding or spotting, which is normal and expected post-procedure. This should stop within a week.
- Avoiding vaginal intercourse, use of tampons, and taking baths until the bleeding has subsided. Showers are okay anytime after the procedure.
Your gynaecologist will see you after your surgery for a follow-up appointment.
Empowering Yourself in Your Health Journey
A hysteroscopy is a minimally invasive procedure that provides a clear view of the uterus, allowing for both diagnosis and treatment of various conditions such as polyps, fibroids, and retained tissue. Whether done under general anesthesia or in a clinic, it offers an effective solution with a generally low risk of complications, though some, like bleeding or uterine perforation, can occur. Recovery is usually quick, and patients can expect to return to normal activities shortly after.
With proper aftercare and follow-up, hysteroscopy serves as a reliable tool in managing uterine health and ensuring a smoother path to recovery.