Table of Contents
- Summary
- Introduction
- What is Pertussis?
- Why Get Vaccinated During Pregnancy?
- When Should You Get the Tdap Vaccine?
- Who is Most Vulnerable to Whooping Cough?
- How Pertussis Spreads
- Symptoms of Pertussis
- General Symptoms
- Severe Complications
- How Common is Pertussis?
- Vaccine Risks
- Common Side Effects
- Rare Side Effects
- Can I Still Get the COVID-19 and Flu Vaccines?
- Do I Still Need Other Vaccines?
Summary:
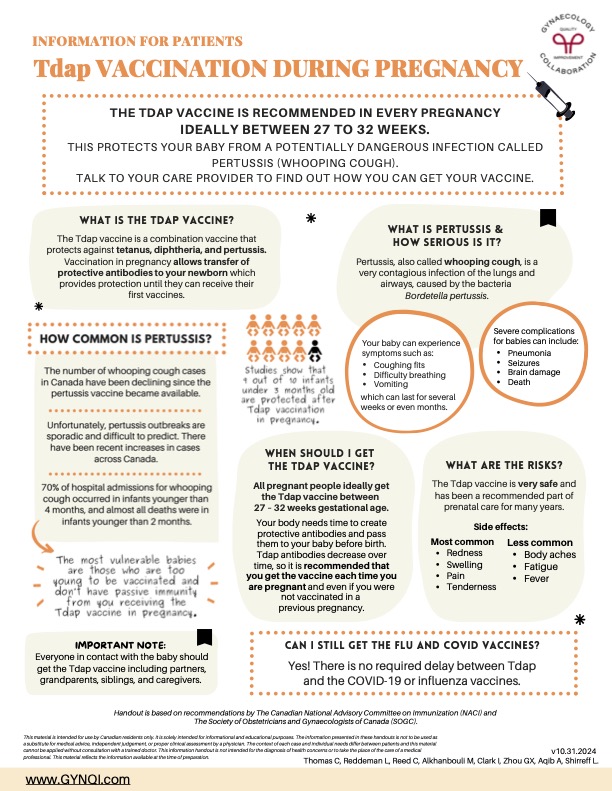
- Pertussis is an infection that can cause symptoms like coughing fits, fever, seizures, pneumonia, and death. It’s caused by the Bordetella pertussis bacteria, which embeds itself into the lining of the respiratory tract and releases toxins.
- In Canada, doctors recommend that all pregnant women get the Tdap vaccine at around 21-32 weeks gestation. This is slightly earlier than the CDC’s standard recommendation of 27-36 weeks.
- While people of all ages can contract whooping cough, infants under two months of age are especially vulnerable to the disease. They are more likely to develop complications like secondary infection.
- The Tdap vaccine is very safe, and in general, the benefits to pregnant mothers and their babies greatly outweigh any risks associated with the injection. Cases of whooping cough are rising, so it is important to get vaccinated for the disease.
The Tdap vaccine is a combination vaccine that protects against tetanus, diphtheria, and pertussis. Getting vaccinated while pregnant transfers protective antibodies to your newborn, which provides protection from all three diseases until they can receive their first vaccines.
Like most other inoculations, the Tdap vaccine is delivered as a quick injection, typically in the upper arm, during a routine office visit. In some provinces, your local pharmacist may also be authorized to administer the vaccine on your doctor’s behalf.
What is Pertussis?
Pertussis, also called whooping cough, is an infection of the lungs and airways caused by a gram-negative bacteria called Bordetella pertussis. It is extremely contagious and can be passed on even when patients are asymptomatic.
Whooping cough gets its name from the distinctive “whooping” sound that occurs after fits of violent coughing. Infants who contract pertussis will often cough for hours at a time and are susceptible to secondary infections like pneumonia.
Bordetella pertussis embeds itself in the lining of the respiratory tract (called cilia), where it releases toxins that trigger severe inflammation and tissue damage. This can result in coughing fits that are severe enough to break ribs and last for weeks or months at a time.
Why Get the Tdap Vaccine During Pregnancy?
Getting the Tdap vaccine is important because 70% of all whooping cough cases that are severe enough to result in hospitalization will occur in an infant under four months of age. Babies younger than two months of age are even more vulnerable.
According to the Centre for Disease Control (CDC), the risk of infants contracting whooping cough before two months of age drops by 78% when pregnant mothers get vaccinated. This makes getting vaccinated the most effective way to protect your baby after birth.
When Should You Get the Tdap Vaccine?
In Canada, doctors recommend that pregnant women receive the Tdap vaccine at some point between weeks 21 and 32 weeks. The mother’s body needs time to create protective antibodies and pass them on to the baby before she gives birth.
Tdap antibodies decrease over time, so it is recommended that you get the vaccine each time you are pregnant. This is true regardless of whether you have been vaccinated in the past or during past pregnancies.
Who is Most Vulnerable to Whooping Cough?
Infants under two months of age are the most vulnerable to whooping cough because their lungs and immune systems haven’t yet fully developed. Since they are too young to be vaccinated, vaccinating the mother during pregnancy is the only way to protect the baby.
While infants are the most vulnerable age group, whooping cough can also be particularly serious for seniors, the immunocompromised, and those with certain pre-existing health conditions, like diabetes, asthma, or COPD.
How Pertussis Spreads
Pertussis usually spreads through droplets in the air when an infected person coughs or sneezes. The total incubation period tends to fall somewhere between 9 to 10 days, but it can last as long as 42 days in some patients.
People who spend time in close contact with the infected or in close quarters like grocery stores, medical clinics, and schools are more likely to contract whooping cough. Isolating at home, especially during a known outbreak, may slightly lower this risk, but isn’t a guarantee.
Part of the problem with pertussis lies in the fact that older patients don’t always develop obvious symptoms right away, especially if they’ve been vaccinated in the past. They may mistake whooping cough for allergies or the common cold.
Symptoms of Pertussis
A person’s age and overall state of health can significantly alter the disease course of whooping cough. In healthy adults and older children, the symptoms often stay mild or may never develop at all because the immune system can fight the bacteria off.
Whooping cough tends to be much more serious in infants. Not only are symptoms generally more severe, but they also can persist for weeks or months at a time.
General Symptoms:
- Coughing Fits
- Difficulty Breathing
- Vomiting (from coughing)
- Low-Grade Fever
Once infected, patients may find it challenging to get enough rest, food, or fluids. This can result in dehydration or malnutrition serious enough to justify hospitalization. Sometimes, IV fluids or parenteral nutrition becomes necessary.
Severe Complications:
- Pneumonia
- Atelectasis
- Hernias
- Seizures
- Encephalopathy
- Brain Damage
- Death
If you or your baby contracts whooping cough in spite of your efforts, it’s important to seek medical attention right away. Taking antibiotics can help reduce the length of the infection and the likelihood of severe complications like these, especially if administered early on.
How Common is Pertussis?
In Canada, the number of whooping cough cases began to decline almost immediately after the pertussis vaccine became available in the 1940s. Whooping cough was a major leading cause of infant deaths before this point.
Unfortunately, pertussis outbreaks are sporadic and can be extremely difficult to predict, especially if patients don’t report their symptoms right away. It is possible for someone to transmit the disease without ever being aware that they had it in the first place.
According to the Public Health Agency of Canada (PHAC), the number of pertussis cases in Canada skyrocketed to 12,000 in the first eight months of 2024. That’s more than double the usual average of 500 to 4,500 cases reported in the years prior.
With case numbers on the rise, getting vaccinated during pregnancy is more important than ever. It is the best way to protect your baby from infection.
Vaccine Risks
The Tdap vaccine is very safe and has been a recommended part of prenatal care for many years. Most people don’t have any issues after the initial pinch associated with the injection itself. However, a small number of people may experience these side effects.
Common Side Effects
- Redness
- Swelling
- Pain
- Tenderness
Rare Side Effects
- Body aches
- Fatigue
- Fever
The pertussis vaccine uses an inactive version of the virus to teach your immune system how to build immunity to it. You cannot contract whooping cough from the vaccine, and any symptoms you develop after vaccination are only a sign that your body is responding appropriately to the medication.
Can I Still Get the COVID-19 and Flu Vaccines?
Yes! There is no need to delay or space out the Tdap, COVID-19, or influenza vaccines. If it’s more convenient for you, ask your doctor to schedule the injections for the same day. What matters most is that you get vaccinated to lower the risk of you and your baby contracting whooping cough or the COVID-19 virus itself.
Do I Still Need Other Vaccines?
Maybe. Health Canada recommends that all pregnant women receive the Tdap, influenza, and COVID-19 vaccines. However, your doctor may also recommend that you get other vaccines if warranted by your situation:
- Pneumococcal Vaccine: If you are immunocompromised or exposed.
- Hepatitis A/B: If you are at risk for contracting either disease.
- Rabies: If you are exposed to rabies or work in a high-risk location.
- Meningitis: If you are immunocompromised or are exposed.
- Typhoid: If you plan to travel to a high-risk area.
- Yellow Fever: If you plan to travel to a high-risk area.
- Malaria: If you plan to travel to a high-risk area.
- RhoGAM: If you have Rh-negative blood.
Your doctor will only recommend vaccines when they feel the benefits for you and your baby outweigh any potential risks. If you have questions or concerns about vaccines, make sure you bring them up during your appointment.



