Table of Contents
- Summary
- Introduction
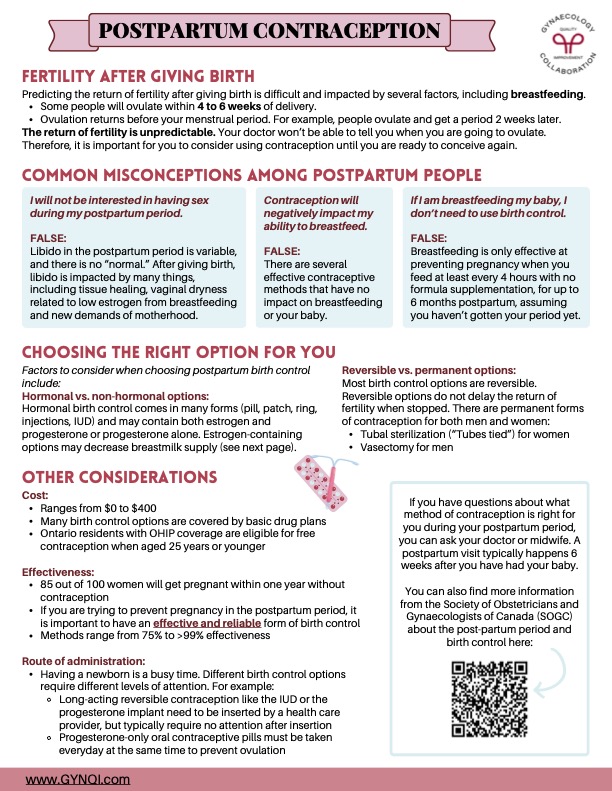
- Fertility After Giving Birth
- Common Misconceptions Among Postpartum Women
- I will not be interested in having sex during my postpartum period
- Contraception will negatively impact my ability to breastfeed
- If I am breastfeeding my baby, I don’t need to use birth control
- Choosing the Right Option For You
- Hormonal vs. Non-Hormonal Options
- Cost
- Effectiveness
- Route of Administration
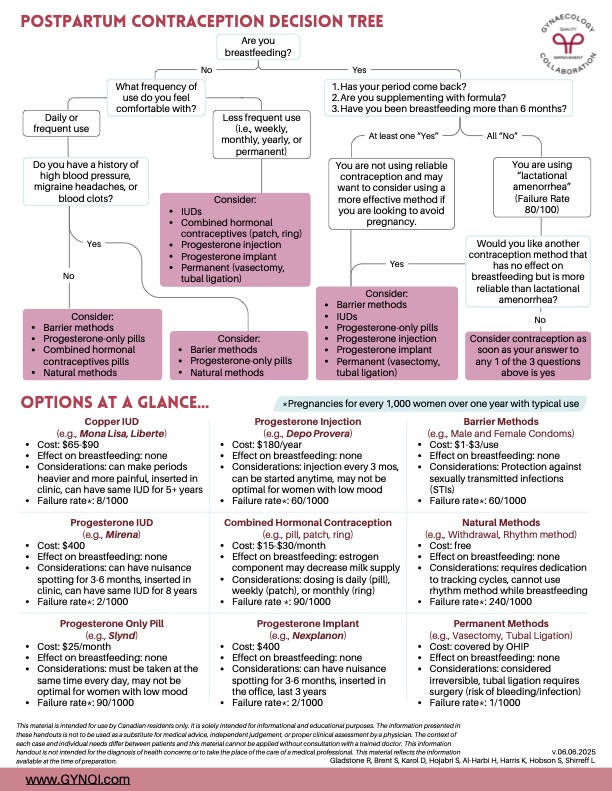
- Your Options At a Glance
- Copper IUD (e.g. Mona Lisa, Liberte)
- Progesterone Injection (e.g. Depo Provera)
- Barrier Methods (e.g. Male and Female Condoms)
- Progesterone IUD (e.g. Mirena)
- Combined Hormonal Contraception (e.g. Pill, Patch, Ring)
- Natural Methods (e.g. Withdrawal, Rhythm Method)
- Progesterone Only Pill (e.g. Micronor)
- Progesterone Implant (e.g. Nexplanon)
- Permanent Methods (e.g. Vasectomy, Tubal Ligation)
- Do You Have More Questions About Birth Control?
Summary:
- Fertility can return at any time after giving birth without warning. It’s important to choose a reliable method of contraception until you’re ready to have another baby.
- There are many misconceptions about fertility after pregnancy. Well-meaning friends and loved ones may unintentionally share methods that aren’t reliable or science-based.
- Some treatments, like estrogen-based birth control pills and IUDs, may slightly reduce milk supply. Others, like progesterone-only pills and barrier methods, won’t affect your ability to nurse your baby at all.
- Your options include the copper IUD, progesterone injection, progesterone-based IUDs, and combination hormones. For women who aren’t interested in medication, condoms, the withdrawal method, and the rhythm method may be acceptable.
Fertility After Giving Birth
Predicting the return of fertility after giving birth is extremely difficult. Your ability to become pregnant can be impacted by a long list of factors, including whether you choose to breastfeed.
- Some women will ovulate within 4 to 6 weeks after delivery.
- Ovulation usually returns before your menstrual period, not the other way around.
- Most women will ovulate, and then start their period around 2 weeks later.
It’s important to note that the return of fertility is always unpredictable. Your doctor won’t be able to tell you when you are going to ovulate, and the people around you might suggest methods of protection that aren’t necessarily rooted in science. That’s why it’s important for you to consider using contraception until you recover or are ready to try to conceive again.
Common Misconceptions Among Postpartum Women
Your body goes through many changes after you give birth. It’s completely natural to feel curious about contraception or have questions about fertility. Understanding your options and dispelling common misconceptions can help you make the best choice for your health and family planning needs.
I will not be interested in having sex during my postpartum period.
FALSE.
Libido in the postpartum period is variable, and there is no “normal.” After giving birth, your desire for sex is impacted by many things, including tissue healing, vaginal dryness related to low estrogen from breastfeeding, and new demands of motherhood.
Contraception will negatively impact my ability to breastfeed.
FALSE.
There are several effective contraceptive methods that have no impact on breastfeeding or your baby. You don’t have to make a choice between one or the other!
If I am breastfeeding my baby, I don’t need to use birth control.
FALSE.
Breastfeeding is only effective at preventing pregnancy when you feed at least every 4 hours with no formula supplementation for up to 6 months postpartum. Because this schedule is so specific, it’s very easy to accidentally trigger ovulation. Plus, if you get your period at any point, it’s a sign that you may be fertile again.
Choosing the Right Option For You
It’s important to find a birth control option that works for you. Your ideal solution won’t necessarily be what works for your sister, mother, or any other woman in your life, and that’s okay! Factors to consider when choosing postpartum birth control include:
Hormonal vs. Non-Hormonal Options
- Hormonal birth control comes in many forms (pill, patch, ring, injections, IUD) and may contain both estrogen and progesterone or progesterone alone. Estrogen-containing options have a higher risk of decreased breast milk supply.
- Non-hormonal options include condoms, copper IUDs, fertility awareness methods, and withdrawal.
Reversible vs. Permanent Options
- Most birth control options are reversible, which means they don’t delay the return of fertility after you stop using them.
- There are permanent forms of contraception for both men and women:
- Tubal Sterilization (Women): Having your fallopian tubes tied or removed.
- Vasectomy (Men) Having the vas deferens tubes cut or tied off.
Cost
- Ranges from $0 to $400
- Many birth control options are covered by basic drug plans
- Ontario residents with OHIP coverage are eligible for free contraception when aged 25 years or younger.
Effectiveness
If you are trying to prevent pregnancy in the postpartum period, it is important to have an effective and reliable form of birth control. 85 out of 100 women will get pregnant within one year without contraception.
- Available methods range from 75% to >99% effectiveness
- The withdrawal method is the least effective.
- Permanent sterilization is the most effective.
Not every form of contraception offers the same level of protection. However, almost all potential options are at least better than using no protection at all.
Route of Administration
Having a newborn is a busy time. Different birth control options require different levels of attention. For example:
- Long-acting reversible contraception like the IUD or the progesterone implant needs to be inserted by a healthcare provider but typically requires no attention after insertion
- Progesterone-only oral contraceptive pills must be taken every day at the same time to prevent ovulation.
Be sure to factor in your lifestyle, the early challenges you might face while parenting a newborn, and your own recovery. Your contraception is more likely to fail if you accidentally forget to use it or overlook it—and that’s more likely to happen when you’re tired or distracted.
Your Options At a Glance
There are many excellent contraception options on the market in Canada. Each offers unique benefits that may make them more or less suitable for you. From the copper IUD to progesterone-only pills, we’ll give you a brief overview of these options next.
Copper IUD (e.g. Mona Lisa, Liberte)
- Cost: $65-$90
- Effect on Breastfeeding: None
- Considerations: Can make periods heavier and more painful, inserted in a clinic, can have the same IUD for 5+ years
- Failure rate1: 8/1000
Progesterone Injection (e.g. Depo Provera)
- Cost: $180/year
- Effect on Breastfeeding: None
- Considerations: Injection every 3 mos, can be started anytime, may not be optimal for women with low mood
- Failure rate1: 60/1000
Barrier Methods (e.g. Male and Female Condoms)
- Cost: $1-$3/use
- Effect on Breastfeeding: None
- Considerations: Protection against sexually transmitted infections (STIs)
- Failure rate1: 200/1000
Progesterone IUD (e.g. Mirena)
- Cost: $400
- Effect on Breastfeeding: None
- Considerations: Can have nuisance spotting for 3-6 months, inserted in a clinic, can have the same IUD for 5 years
- Failure rate1: 2/1000
Combined Hormonal Contraception (e.g. Pill, Patch, Ring)
- Cost: $15-$30/month
- Effect on Breastfeeding: Estrogen component may decrease milk supply
- Considerations: Dosing is daily (pill), weekly (patch) or monthly (ring)
- Failure rate1: 90/1000
Natural Methods (e.g. Withdrawal, Rhythm Method)
- Cost: Free
- Effect on Breastfeeding: None
- Considerations: Requires dedication to tracking cycles, cannot use rhythm method while breastfeeding
- Failure rate1: 240/1000
Progesterone Only Pill (e.g. Micronor)
- Cost: $15-$30/month
- Effect on Breastfeeding: None
- Considerations: Must be taken at the same time every day, may not be optimal for women with low mood
- Failure rate1: 90/1000
Progesterone Implant (e.g. Nexplanon)
- Cost: $400
- Effect on Breastfeeding: None
- Considerations: Can have nuisance spotting for 3-6 months, inserted in the office, lasts 3 years
- Failure rate1: 2/1000
Permanent Methods (e.g. Vasectomy, Tubal Ligation)
- Cost: Covered by OHIP
- Effect on Breastfeeding: None
- Considerations: Considered irreversible, tubal ligation requires surgery (risk of bleeding and infection)
- Failure rate1: 1/1000
Do You Have More Questions About Birth Control?
If you have questions about what method of contraception is right for you during your postpartum period, you can ask your doctor or midwife. A postpartum visit typically happens 6 weeks after you have had your baby.
You can also get more information about the post-partum period and birth control from the Society of Obstetricians and Gynaecologists of Canada (SOGC).
1All stated pregnancy rates are per every 1,000 women over one year with typical use.



