
Table of Contents
- Summary
- What is Dyspareunia?
- Categorizing Dyspareunia
- Impact of Dyspareunia
- Causes of Dyspareunia
- Biological
- Psychological
- Relational
- Sociocultural
- Assessment of Dyspareunia
- Diagnosing Dyspareunia
- Treating Dyspareunia
- Staying Informed About Your Well-Being
Summary:
- Dyspareunia is characterized by pelvic pain during sexual activity, affecting up to 20% of women and trans individuals across all age groups, manifesting as discomfort during penetrative intercourse or digital stimulation.
- The condition can be categorized into various types, including superficial vs. deep pain, primary (existing from the first sexual experience) vs. secondary (developing after previously pain-free experiences), and generalized (occurring in different situations) vs. situational (specific to certain partners or encounters).
- Dyspareunia can lead to significant emotional stress, social isolation, decreased sexual interest, and relationship issues, with contributing factors ranging from biological (like infections and hormonal changes) to psychological and sociocultural influences.
- If experiencing dyspareunia, individuals should consult a healthcare provider for a thorough assessment, which may include physical exams and psychological evaluations. Treatment options vary and can include pelvic floor physiotherapy, psychotherapy, lubricants, medical therapy, and more, tailored to address the multifactorial nature of the pain.
Dyspareunia is characterized by pelvic pain during sexual activity, often manifesting as discomfort during penetrative intercourse or digital stimulation. This condition can affect up to 20% of women and trans individuals across all age groups. Dyspareunia is categorized into various types, such as superficial or deep pain, primary or secondary onset, and generalized or situational experiences. By recognizing these categories, individuals can better navigate the complexities of dyspareunia and its impact on their sexual health and relationships.
What is Dyspareunia?
Dyspareunia is defined as pelvic pain during sexual activity, commonly experienced as discomfort during penetrative intercourse or digital stimulation. It can affect up to 20% of women and trans people of all ages.
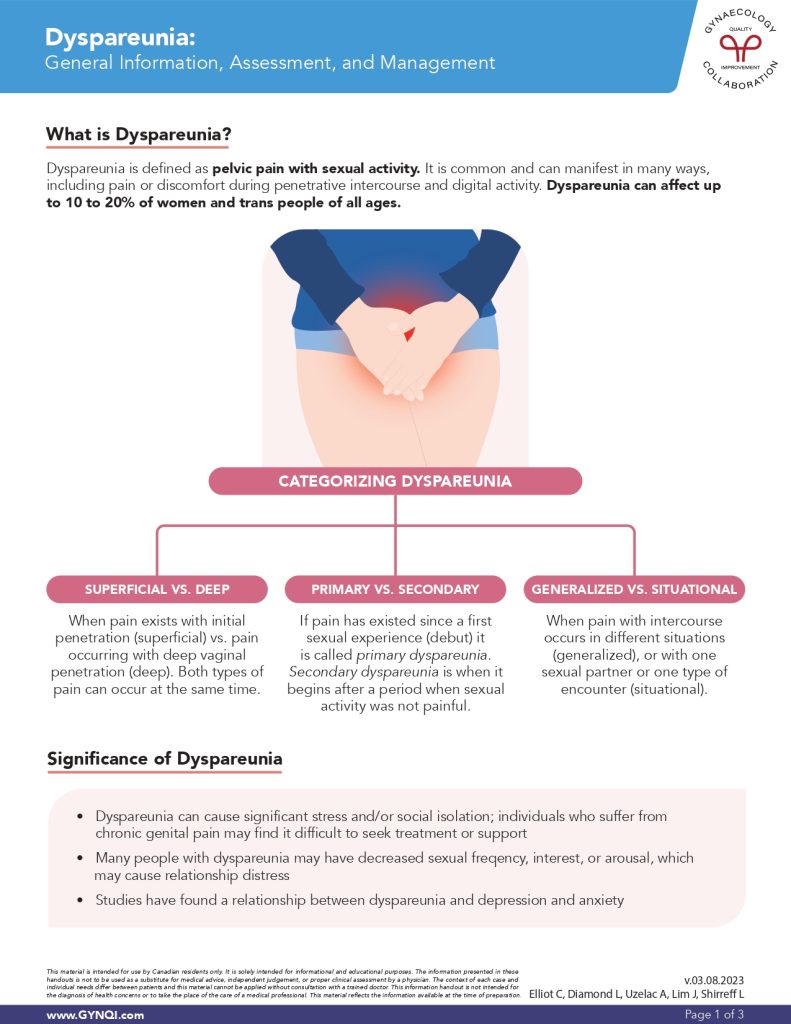
Categorizing Dyspareunia
Dyspareunia can be categorized based on various factors. These categories include:
Superficial vs. Deep: Pain occurs with initial (superficial) penetration or with deep vaginal penetration. Both types can occur simultaneously.
Primary vs. Secondary: If pain has existed since a first sexual experience (debut) it is called primary dyspareunia. Secondary dyspareunia is when pain begins after a period when sexual activity was not painful.
Generalized vs. Situational: When pain with intercourse occurs in different situations (generalized), or with one sexual partner or one type of encounter (situational).
Impact of Dyspareunia
Dyspareunia can lead to considerable stress and social isolation, making it challenging for individuals with chronic genital pain to seek treatment or support. Many experience decreased sexual frequency, interest, or arousal, potentially causing relationship distress. Additionally, studies have identified a link between dyspareunia and increased rates of depression and anxiety.
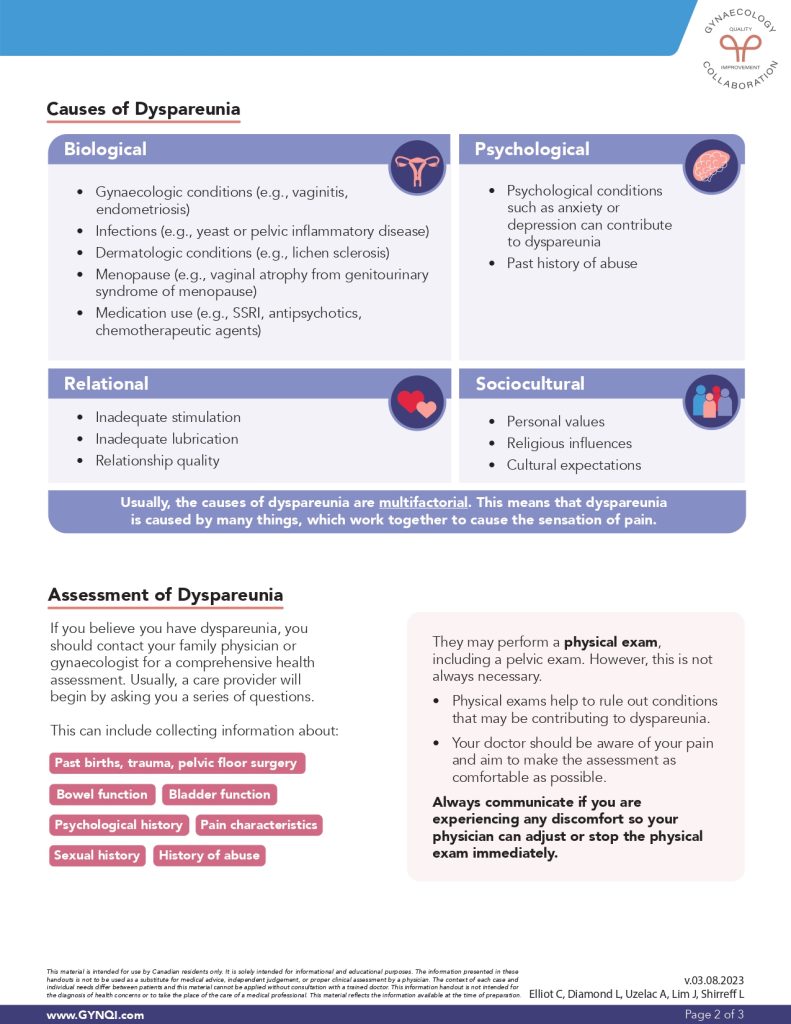
Causes of Dyspareunia
Dyspareunia is typically multifactorial, meaning it is the result of a combination of factors that contribute to the experience of pain.
Biological
Biological causes of Dyspareunia can include:
- Gynaecological conditions (e.g., vaginitis, endometriosis)
- Infections (e.g., yeast or pelvic inflammatory disease)
- Dermatologic conditions (e.g., lichen sclerosus)
- Menopause (e.g., vaginal atrophy from genitourinary syndrome of menopause)
- Medication use (e.g., SSRI, antipsychotics, chemotherapeutic agents)
Psychological
Anxiety, depression, and other psychological disorders can contribute to dyspareunia, along with a past history of abuse.
Relational
Relational issues may contribute to dyspareunia due to the emotional and psychological stress they create. Potential causes of dyspareunia can also consist of inadequate stimulation and lubrication, and the overall quality of your relationship.
Sociocultural
Sociocultural issues can contribute to dyspareunia by shaping beliefs, attitudes, and expectations around sexuality. Personal values, religious influences, and cultural expectations can all lead to dyspareunia.
Assessment of Dyspareunia
If you believe you have dyspareunia, you should contact your family physician or gynaecologist for a comprehensive health assessment. Usually, a care provider will begin the assessment by asking you a series of questions. These can include:
- Past births, trauma, and pelvic floor surgery
- Bowel function
- Bladder function
- Psychological history
- History of abuse
- Pain characteristics
- Sexual history
Diagnosing Dyspareunia
Your doctor may perform a physical exam, including a pelvic exam. However, this is not always necessary. Physical exams help to rule out conditions that may be contributing to dyspareunia.
It is important that your doctor is made aware of your pain and should aim to make the assessment as comfortable as possible. Always communicate if you are experiencing any discomfort so they can adjust or stop the physical exam immediately.
Treating Dyspareunia
Treatment options and management of dyspareunia vary based on the cause, and since dyspareunia is often multifactorial, a comprehensive and multi-faceted approach may be necessary.
Treatment options include:
Pelvic Floor Physiotherapy: Often, the goal is to strengthen and relax the pelvic floor muscles to allow for entry into the vaginal canal as well as retrain pain receptors. This is done over many weeks.
Psychotherapy: This may address a history of abuse or psychological conditions that are contributing to dyspareunia.
- Cognitive Behaviour Therapy can be done to focus on the thinking patterns associated with pain and fear, the emotions associated with these thoughts, and the subsequent behaviours these thoughts and emotions may cause.
Lubricants: Products such as coconut oil can lubricate the vaginal canal, decreasing friction upon vaginal entry.
Moisturizers: Moisturizers differ from lubricants because they bind to water molecules, creating a film-like barrier that may potentially last longer than a lubricant.
Anaesthetics: For pain upon entry, the application of topical lidocaine around the vaginal entrance can help numb the area to allow for penetration or stimulation. It is important that a cis-male sexual partner wear a condom to prevent de-sensitization of their genitals.
Medical Therapy: For women with vaginal dryness caused by low estrogen, local estrogens may help with symptoms of dryness and irritation. Other medications such as steroids, antibiotics, and antifungals depend on the cause of dyspareunia.
Options such as surgery or Botox injections are unusual and not typically recommended but may be an option depending on the primary cause.
Staying Informed About Your Well-Being
Dyspareunia, or pelvic pain during sexual activity, is a common condition that can significantly affect individuals’ sexual health and relationships. Addressing the multifactorial nature of dyspareunia through a comprehensive management plan can lead to improved well-being and a more satisfying sexual experience for those affected. If you are experiencing pain and discomfort, speak to your doctor about your treatment options, and start your path toward feeling your absolute best.



