Induction Of Labour
In most pregnancies, labour starts naturally between 37 and 42 weeks. Sometimes, the health care team thinks it is safer for the birthing parent, fetus, or both to start the process of labour sooner. Induction of labor (IOL) refers to the medical initiation of labour before the onset of spontaneous labour.
‘Labour augmentation‘ refers to using similar medications to continue spontaneous labour when the progression has slowed down or stopped.
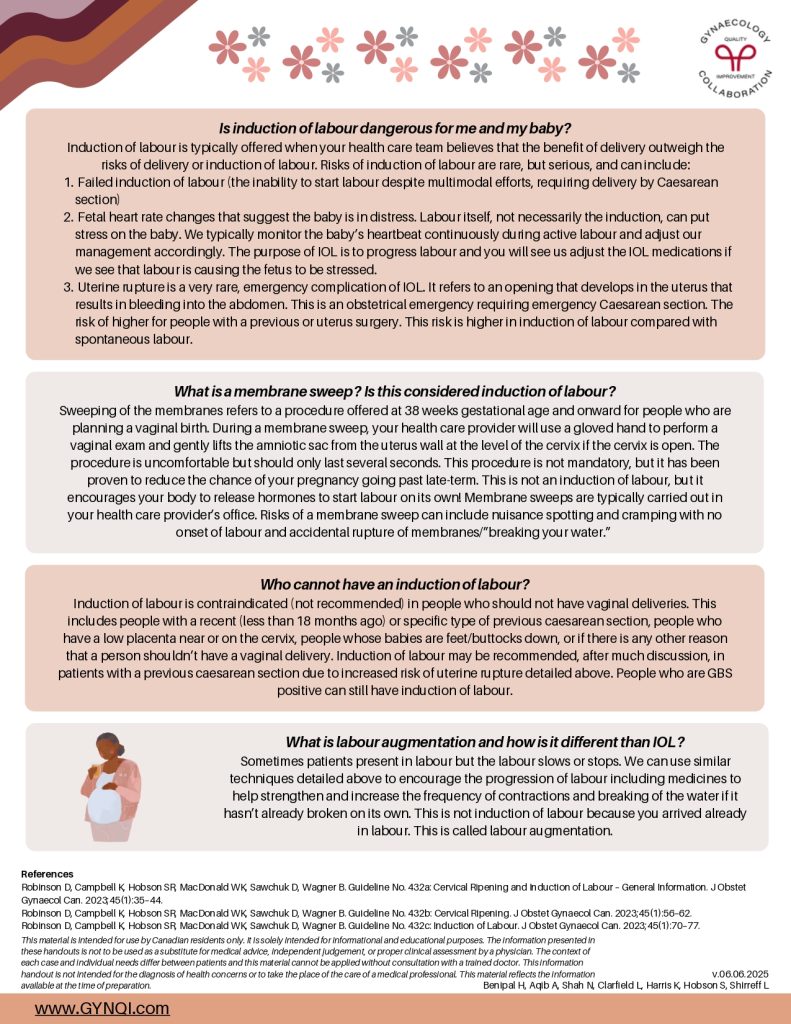
Examples of reasons labour may be induced include:
- Post-dates pregnancy (41-42 weeks gestation)
- High blood pressure in pregnancy
- Placental concerns affecting pregnancy
- Prelabour rupture of membranes (PROM; your water breaks but labour does not start)
- Other health concerns causing unsafe pregnancy
- Uterine infection
- Concerns with baby’s wellbeing
- Decrease in amniotic fluid
- IVF pregnancies
- Gestational diabetes mellitus
What Happens During Induction of Labour?
Step 1: Getting Your Cervix Ready For Labour
IOL starts with a cervical exam to see if your cervix is ready (open/thin/soft enough) for step 2 of the process (labour). Most first-time pregnant people and many second-time pregnant people need cervical ripening prior to step 2. If needed, cervical ripening is typically started in one of two ways:
Option 1: Foley Catheter
- The most common method of cervical ripening is with a foley catheter. This is where we use a speculum or a gloved hand to insert a thin tube into the cervix and inflate a balloon at the end of the tube to put mechanical pressure on the cervix to encourage it to dilate.
- The procedure is uncomfortable and can take anywhere between thirty seconds to several minutes. You may experience a bit of spotting with catheter insertion.
- Once the catheter is inserted, we monitor the baby’s heart rate.
- Unless otherwise recommended/scheduled, you are then typically discharged home from hospital. The catheter is left in place between 12 and 24 hours. The team will give you instructions on when to call/return to hospital.
- Once the catheter falls out, we know that you are at least ~3cm dilated! Only 7 more cm to go!
Option 2: Medication
Medications called prostaglandins can be used instead to encourage the cervix to open and become softer/thinner. This medication can be in the form of:
- An insert (looks similar to a tampon) and is inserted and left inside the vagina for 12-24 hours.
- A gel (inserted into the vagina using an applicator) and works over 6 hours.
- A pill (either swallowed by mouth or inserted into the vagina) that is taken every few hours.
Hospitals have different protocols regarding fetal monitoring before and after your cervical ripening. You should expect to be in the hospital for several hours!
Step 2: Starting Your Contractions
Now you are ready for the onset of labour. We do this in two ways.
1) Medication
We will start one of two medications to start or continue contractions.
Misoprostol is a type of prostaglandin that is given to the patient, usually by mouth, every 2-4 hours. It works to both soften the cervix and start contractions. Throughout labour, we will adjust the dosing and timing of the medicine based on the progress of labour and the strength and frequency of your contractions.
Oxytocin is a hormone your body makes that binds to uterine receptors to produce contractions. We can give you the body-identical hormone through the intravenous to help start or continue contractions.
2) Amniotomy (breaking of the waters)
- If your waters are not broken, we can help the progress of labour by breaking the waters for you. This is done through a vaginal exam where a small plastic instrument called an amnihook is used to make a small hole in the sac around the baby, allowing the fluid to leak out.
- The procedure can be uncomfortable, particularly for people without an epidural but typically lasts only seconds.
- There are no nerve endings on the sac for yourself or your baby, so it does not hurt either of you.
- Your baby continues to produce amniotic fluid, so you will continue to leak fluid up until the delivery of your baby.
- Your health care provider will make sure the presenting part of the baby is low enough before the water is broken. This minimizes the risk of the wrong part of the pregnancy (e.g., baby part other than head or umbilical cord) coming through the cervix.
Common Induction of Labour Questions and Answers
How long does induction of labour take?
It is normal for induction of labour to take anywhere from 1-3 days. Induction of labour takes longer if it is your first time delivery and/or if you require cervical ripening (i.e., ‘Step 1′ described above). Depending on where you are delivering, you will typically be scheduled for a day and time for your induction of labour. The labour floor can be unpredictably busy or quiet and you may get a call to delay your induction of labour to ensure we have the appropriate staffing and rooms available to keep you, your baby, and all other labouring people safe!
Am I in the hospital for the whole induction of labour?
Speak to your health care provider about whether you are booked for an outpatient or inpatient induction of labour. After we do fetal monitoring, most people will be sent home after Step 1 (cervical ripening) if it is safe for the person and baby to do so. Depending on the hospital, you will be given a time to call the labour floor or to return to the labour floor for the remainder of your induction of labour. Remember, the labour floor is available to you 24 hours / day so you can return at any time if you have concerns including, but not limited to: 1) if you think your water broke; 2) heavy vaginal bleeding; 3) if you are worried about changes in your baby’s movements; or 4) if contractions start and are getting too intense to manage at home.
Does induction of labour increase my chances of needing a Caesarean section?
No! IOL does not increase your chance of needing a C-section.
Is induction of labour dangerous for me and my baby?
Induction of labour is typically offered when your health care team believes that the benefit of delivery outweigh the risks of delivery or induction of labour. Risks of induction of labour are rare, but serious, and can include:
- Failed induction of labour (the inability to start labour despite multimodal efforts, requiring delivery by Caesarean section)
- Fetal heart rate changes that suggest the baby is in distress. Labour itself, not necessarily the induction, can put stress on the baby. We typically monitor the baby’s heartbeat continuously during active labour and adjust our management accordingly. The purpose of IOL is to progress labour and you will see us adjust the IOL medications if we see that labour is causing the fetus to be stressed.
- Uterine rupture is a very rare, emergency complication of IOL. It refers to an opening that develops in the uterus that results in bleeding into the abdomen. This is an obstetrical emergency requiring emergency Caesarean section. The risk of higher for people with a previous or uterus surgery. This risk is higher in induction of labour compared with spontaneous labour.
What is a membrane sweep? Is this considered induction of labour?
Sweeping of the membranes refers to a procedure offered at 38 weeks gestational age and onward for people who are planning a vaginal birth. During a membrane sweep, your health care provider will use a gloved hand to perform a vaginal exam and gently lifts the amniotic sac from the uterus wall at the level of the cervix if the cervix is open. The procedure is uncomfortable but should only last several seconds. This procedure is not mandatory, but it has been proven to reduce the chance of your pregnancy going past late-term. This is not an induction of labour, but it encourages your body to release hormones to start labour on its own! Membrane sweeps are typically carried out in your health care provider’s office. Risks of a membrane sweep can include nuisance spotting and cramping with no onset of labour and accidental rupture of membranes/”breaking your water.”
Who cannot have an induction of labour?
Induction of labour is contraindicated (not recommended) in people who should not have vaginal deliveries. This includes people with a recent (less than 18 months ago) or specific type of previous caesarean section, people who have a low placenta near or on the cervix, people whose babies are feet/buttocks down, or if there is any other reason that a person shouldn’t have a vaginal delivery. Induction of labour may be recommended, after much discussion, in patients with a previous caesarean section due to increased risk of uterine rupture detailed above. People who are GBS positive can still have induction of labour.
What is labour augmentation and how is it different than IOL?
Sometimes patients present in labour but the labour slows or stops. We can use similar techniques detailed above to encourage the progression of labour including medicines to help strengthen and increase the frequency of contractions and breaking of the water if it hasn’t already broken on its own. This is not induction of labour because you arrived already in labour. This is called labour augmentation.