Perineal Lacerations
The perineum is the area between the opening to the vagina and anus. Perineal (“pear-uh-NEE-al”) lacerations, also called obstetrical tears, occur in about 85% of vaginal births. They are more common in a someone’s first delivery. There are several types of perineal lacerations.
Types of Perineal Lacerations
Although less common, there can be tears on the labia (upper parts of the vaginal opening), near the urethra (the hole you pee from), or your clitoris.
We grade perineal lacerations based on what anatomical structures they involve, rather than the size and/or “how many stitches” are involved.
1st Degree
Tear of the perineal skin/lining of vagina only.
2nd Degree
Tear of the perineal skin/lining of vagina and perineal muscles. This is the most common type of perineal laceration.
3rd Degree
Tear of the perineal skin/lining of vagina, perineal muscles, and muscles around the anus (anal sphincter).
4th Degree
Tear of the perineal skin/lining of vagina, perineal muscles, anal sphincter, and lining of the anus/rectum.
Obstetrical Anal Sphincter Injury (OASIS)
These are more extensive tears that have traditionally been called ‘third- and fourth-degree’ tears.
What Is an Episiotomy?
An episiotomy is a cut made by your health care provider into the vaginal wall and perineum to make more space for your baby to be delivered.
Episiotomies are typically offered if your baby needs to be born quickly or if you are at risk of a serious perineal tear. They are done with your consent.
For more information, see our handout “An Overview of Episiotomy.”
Diagnosis & Treatment of Perineal Lacerations
After the birth of your baby, your health care provider will carefully examine your vagina, perineum, and rectum to determine if you have a tear and what structures are involved.
If you have had a tear or an episiotomy, your health care provider will typically begin to repair the area using dissolvable stitches.
For more information about OASIS, please see the Sinai Health OASIS Clinic website: https://www.sinaihealth.ca/areas-of-care/wih/gynaecology/mount-sinai-perineal-oasis-clinic
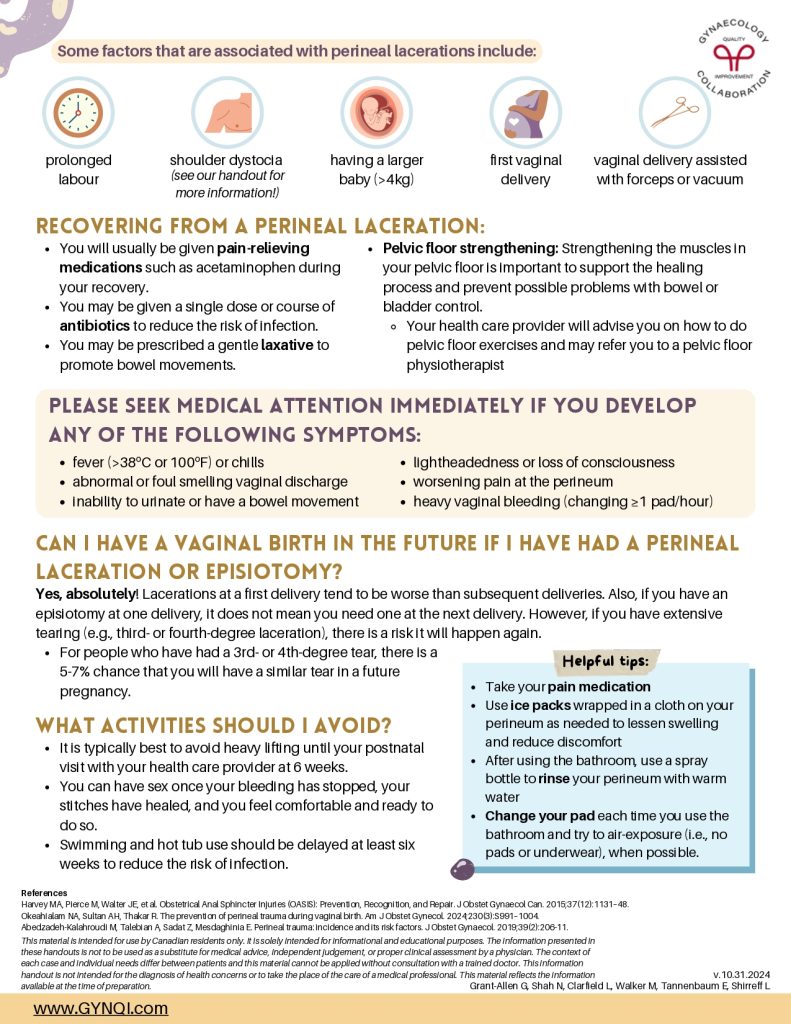
Some factors that are associated with perineal lacerations include:
- Prolonged labour
- Shoulder dystocia (see our handout for more information)
- Having a larger baby (>4kg)
- First vaginal delivery
- Vaginal delivery assisted with forceps or vacuum
Recovering From A Perineal Laceration
- You will usually be given pain-relieving medications such as acetaminophen during your recovery.
- You may be given a single dose or course of antibiotics to reduce the risk of infection.
- You may be prescribed a gentle laxative to promote bowel movements.
- Pelvic floor strengthening: Strengthening the muscles in your pelvic floor is important to support the healing process and prevent possible problems with bowel or bladder control.
- Your health care provider will advise you on how to do pelvic floor exercises and may refer you to a pelvic floor physiotherapist
Please Seek Medical Attention Immediately If You Develop Any of the Following Symptoms:
- fever (>38ºC or 100ºF) or chills
- abnormal or foul smelling vaginal discharge
- inability to urinate or have a bowel movement
- lightheadedness or loss of consciousness
- worsening pain at the perineum
- heavy vaginal bleeding (changing ≥1 pad/hour)
Can I Have A Vaginal Birth in the Future If I Have Had A Perineal Laceration or Episiotomy?
Yes, absolutely! Lacerations at a first delivery tend to be worse than subsequent deliveries. Also, if you have an episiotomy at one delivery, it does not mean you need one at the next delivery. However, if you have extensive tearing (e.g., third- or fourth-degree laceration), there is a risk it will happen again.
- For people who have had a 3rd- or 4th- degree tear, there is a 5-7% chance that you will have a similar tear in a future pregnancy.
What Activities Should I Avoid?
- It is typically best to avoid heavy lifting until your postnatal visit with your health care provider at 6 weeks.
- You can have sex once your bleeding has stopped, your stitches have healed, and you feel comfortable and ready to do so.
- Swimming and hot tub use should be delayed at least six weeks to reduce the risk of infection.
Helpful Tips
- Take your pain medication
- Use ice packs wrapped in a cloth on your perineum as needed to lessen swelling and reduce discomfort
- After using the bathroom, use a spray bottle to rinse your perineum with warm water
Change your pad each time you use the bathroom and try to air-exposure (i.e., no pads or underwear), when possible.