Breech Presentation
Near the end of pregnancy, babies usually position themselves to be head down so that the head will come out of the vagina first. This is called “cephalic presentation.“ Breech presentation happens when your baby’s “presenting part”, meaning the part of the baby closest to your cervix, is the baby’s buttocks or feet.
While it can be common for babies to be in this position throughout pregnancy, only 3-4% of fetuses will be in breech position at term (37 weeks). Sometimes, there is no cause for a breech presentation, but there are several things that increase the risk of having a breech baby.
Risk Factors For Breech Presentation
- Premature (i.e., pregnancy less than 37 weeks)
- Uterine malformations (e.g., bicornuate uterus)
- Too much or too little amniotic fluid around the baby
- Multiple gestation (e.g., twins or triplets)
- Uterine fibroids
- Placenta previa or low lying placenta
- Fetal anomalies
Why Does It Matter If A Baby Is Born In Breech Position?
Breech presentation has implications for the mode of delivery of the baby (e.g., vaginal delivery or Caesarean delivery), and for the baby, regardless of how they are delivered.
Regardless of the mode of delivery, babies who were in breech position right before delivery do have higher risk of some conditions including torticollis (stiffening of your baby’s neck muscles, causing their head to tilt to one side) and development of dysplasia of the hip.
Types of Breech Position
Complete Breech (the baby’s hips and knees are flexed)
Incomplete Breech (the hip and knee of one of the baby’s limbs are flexed incompletely)
Frank Breech (the baby’s hips are flexed and their knees are extended)
How Are Breech Babies Delivered?
Compared to a baby who is head down (cephalic presentation), vaginal delivery of a breech baby can increase the risk of serious complications at birth (see below). Vaginal breech delivery is performed commonly for a second twin in a twin pregnancy. However, vaginal breech delivery for a singleton pregnancy is uncommon in Canada.
Planned Caesarean section avoids most of this risk and this is offered as the first-line and safest mode of delivery(see below). External cephalic version (ECV) is a procedure to try to turn the baby head down to avoid Caesarean section in eligible candidates (see next page).
Elective Caesarean Birth
An elective Caesarean section is a planned surgery to remove the fetus from the birthing parent’s abdomen. This is not risk-free but is typically considered safer for the birthing person and baby, in Canada, if the baby is in breech presentation.
This is usually booked around 39 weeks gestational age, but you will have a conversation with your obstetrician about the right time for you. The surgery will be done sooner for you if you go into labour prior to your booked surgery date.
Please see our handout “All About Caesarean Sections” for more information.
Vaginal Breech Birth
Except for with twins, where this is commonly done for the 2nd twin in some people, vaginal breech delivery is quite rare in Canada. While it is an option in highly-selected patients, vaginal delivery puts you and your baby at higher risk for:
- fetal fractures and/or dislocations
- dystocia (the baby getting stuck)
- fetal asphyxia (low oxygen)
- fetal limb prolapse
- umbilical cord prolapse
- fetal death
- increased tearing and/or damage to the vagina and cervix of the delivering person
Providers strongly recommend against a vaginal breech birth if:
- the umbilical cord is the presenting part below the baby
- the baby is predicted to be very small or very big
- the baby’s feet are presenting below the baby’s bum
- there is a fetal anomaly that may interfere with vaginal delivery
- the fetal head is hyperextended (looking far back)
External Cephalic Version (ECV)
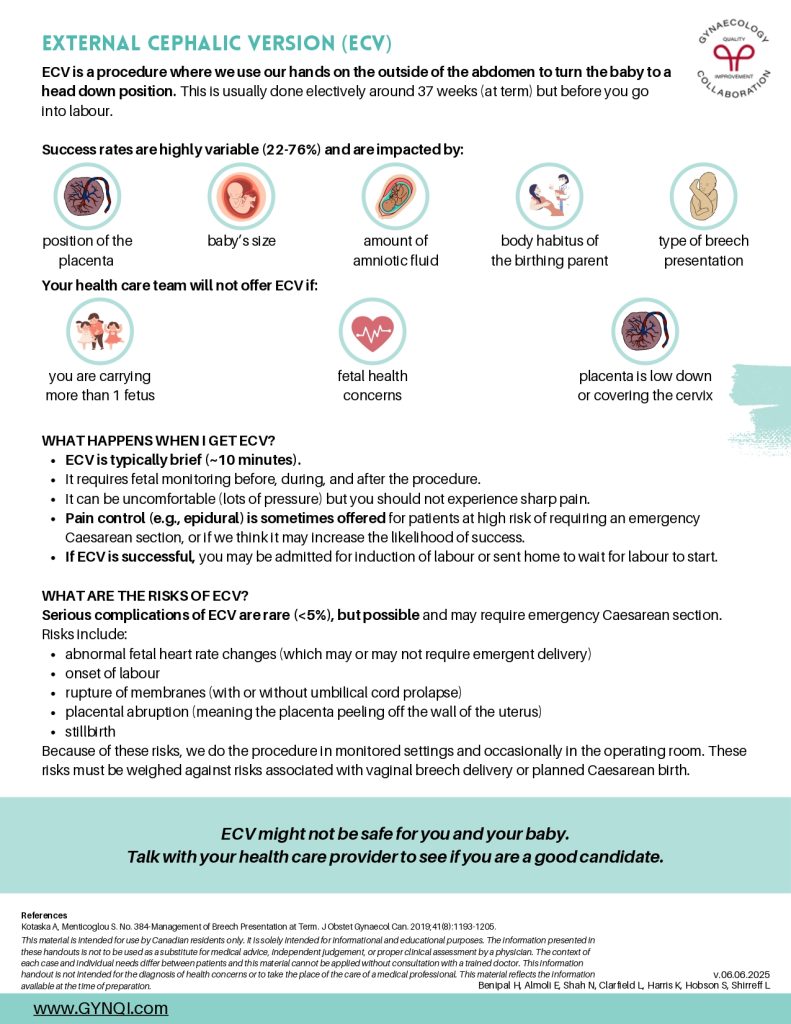
ECV is a procedure where we use our hands on the outside of the abdomen to turn the baby to a head down position. This is usually done electively around 37 weeks (at term) but before you go into labour.
Success rates are highly variable (22-76%) and are impacted by:
- Position of the placenta
- Baby’s size
- Amount of amniotic fluid
- Body habitus of the birthing parent
- Type of breech presentation
Your health care team will not offer ECV if:
- You are carrying more than 1 fetus
- Fetal health concerns
- Placenta is low down or covering the cervix
What Happens When I Get Ecv?
- ECV is typically brief (~10 minutes).
- It requires fetal monitoring before, during, and after the procedure.
- It can be uncomfortable (lots of pressure) but you should not experience sharp pain.
- Pain control (e.g., epidural) is sometimes offered for patients at high risk of requiring an emergency Caesarean section, or if we think it may increase the likelihood of success.
- If ECV is successful, you may be admitted for induction of labour or sent home to wait for labour to start.
What Are The Risks Of Ecv?
Serious complications of ECV are rare (<5%), but possible and may require emergency Caesarean section. Risks include:
- abnormal fetal heart rate changes (which may or may not require emergent delivery)
- onset of labour
- rupture of membranes (with or without umbilical cord prolapse)
- placental abruption (meaning the placenta peeling off the wall of the uterus)
- stillbirth
Because of these risks, we do the procedure in monitored settings and occasionally in the operating room. These risks must be weighed against risks associated with vaginal breech delivery or planned Caesarean birth.
ECV might not be safe for you and your baby. Talk with your health care provider to see if you are a good candidate.