Postpartum Hemorrhage
What Is Postpartum Hemorrhage?
Some bleeding after delivery is considered normal. Postpartum hemorrhage (PPH) occurs when the individual who has given birth (either via Caesarean or vaginal delivery) is bleeding more than is typically expected after delivery. It is medically defined as maternal blood loss over 500ml (vaginal delivery) or 1000ml (Caesarean delivery), or if the patient develops signs of hypovolemia (low blood volume) after delivery. Postpartum hemorrhage occurs in 3-5% of deliveries and can range in severity. It can happen immediately after delivery or within the first 6 weeks of the postpartum time.
Causes of Postpartum Hemorrhage
There are many risk factors for and causes of postpartum hemorrhage that can largely be grouped into “4 Ts”.
| Cause | Explanation |
| Tone (uterine atony) | Normally, the uterus contracts after delivery to stop maternal bleeding. Low tone of the uterus, often referred to as uterine atony, means it isn’t contracting properly to stop bleeding. There are certain things that put you at higher risk for this including developing an infection in labour, having twins, or having a fast labour. Low uterine tone after a delivery is the most common cause of PPH. |
| Trauma (surgical bleeding or tearing) | Vaginal lacerations/tears or surgical bleeding (i.e., at C-section) that occur during delivery or uterine rupture can also cause PPH. |
| Tissue (retained piece of placenta) | The placenta is delivered after the baby. Sometimes, a small piece of the placenta fails to detach from the uterus and is left inside, which can lead to a PPH. This is sometimes called “retained products of conception” (RPOC). |
| Thrombin (medical word for a protein related to bleeding) | If an individual has or develops a blood clotting-factor deficiency, this can cause them to bleed more after delivery. This is a more uncommon cause of PPH. |
Iron Deficiency Anemia In Pregnancy
Anemia (when your body doesn’t have enough red blood cells) is common in pregnancy. Anemia can happen for a number of reasons, but is most commonly caused by a deficiency of iron, which is a ‘building block’ of red blood cells. Part of why we take anemia so seriously in pregnancy is that patients who are anemic are more likely to become unwell from postpartum bleeding. Our handout, “You Have Iron Deficiency (And You’re Pregnant)“, has more details about anemia during pregnancy and its treatment.
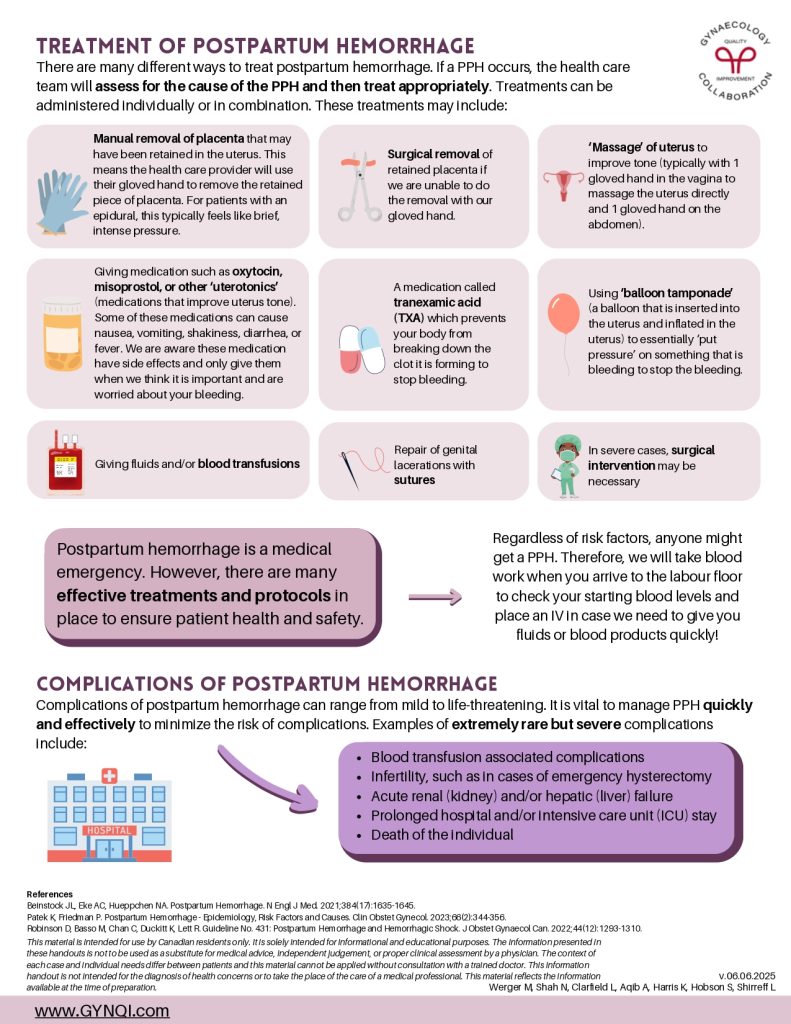
Treatment of Postpartum Hemorrhage
There are many different ways to treat postpartum hemorrhage. If a PPH occurs, the health care team will assess for the cause of the PPH and then treat appropriately. Treatments can be administered individually or in combination. These treatments may include:
- Manual removal of placenta that may have been retained in the uterus. This means the health care provider will use their gloved hand to remove the retained piece of placenta. For patients with an epidural, this typically feels like brief, intense pressure.
- Giving medication such as oxytocin, misoprostol, or other ‘uterotonics’ (medications that improve uterus tone). Some of these medications can cause nausea, vomiting, shakiness, diarrhea, or fever. We are aware these medication have side effects and only give them when we think it is important and are worried about your bleeding.
- A medication called tranexamic acid (TXA) which prevents your body from breaking down the clot it is forming to stop bleeding.
- Surgical removal of retained placenta if we are unable to do the removal with our gloved hand.
- ‘Massage’ of uterus to improve tone (typically with 1 gloved hand in the vagina to massage the uterus directly and 1 gloved hand on the abdomen).
- Using ‘balloon tamponade’ (a balloon that is inserted into the uterus and inflated in the uterus) to essentially ‘put pressure’ on something that is bleeding to stop the bleeding.
- Giving fluids and/or blood transfusions
- Repair of genital lacerations with sutures
- In severe cases, surgical intervention may be necessary
Postpartum hemorrhage is a medical emergency. However, there are many effective treatments and protocols in place to ensure patient health and safety.
Regardless of risk factors, anyone might get a PPH. Therefore, we will take blood work when you arrive to the labour floor to check your starting blood levels and place an IV in case we need to give you fluids or blood products quickly!
Complications of Postpartum Hemorrhage
Complications of postpartum hemorrhage can range from mild to life-threatening. It is vital to manage PPH quickly and effectively to minimize the risk of complications. Examples of extremely rare but severe complications include:
- Blood transfusion associated complications
- Infertility, such as in cases of emergency hysterectomy
- Acute renal (kidney) and/or hepatic (liver) failure
- Prolonged hospital and/or intensive care unit (ICU) stay
- Death of the individual