Table of Contents
- Summary
- Introduction
- Getting to Know Assisted Vaginal Birth
- What Are the Different Types of AVB?
- The Goal of an Assisted Birth
- When Doctors Recommend AVB
- What does an AVB Mean for Future Pregnancies?
- What Are the Risks of an AVB?
- Extra Procedures
- Recovering From an AVB
- AVB and Your Mental Health
Summary:
- Labor and birth can be unpredictable. In a small percentage of births, doctors may need to step in and use forceps or a vacuum device to help deliver the baby—this is called an Assisted Vaginal Birth (AVB).
- Your doctor will only recommend an AVB if they are sure it is the best way to keep you and your baby safe while ensuring successful delivery. Asking questions about this process in advance can help you feel more in control.
- Forceps and vacuum deliveries do carry certain risks, although these risks are often lower than those associated with a c-section. You may also need additional procedures to facilitate AVB, such as an episiotomy or manual rotation of your baby.
- Having an AVB can slightly lengthen your recovery time after birth, and you may struggle with difficult emotions along the way. It’s completely normal to respond with anxiety, sadness, or even anger—your doctor can help you find ways to manage.
Assisted Vaginal Birth (AVB) typically involves using forceps or a vacuum suction device to gently guide the baby down the vaginal canal during pushing. This procedure can help labouring mothers deliver without the need for a Caesarean section (C-section), and may sometimes be the only safe option.
If you’re preparing to deliver your baby, or your doctor has informed you that you will likely need an AVB, you may be experiencing a mixture of feelings about it, including anxiety. Getting to know how an AVB happens and why can help you feel more confident and in control.
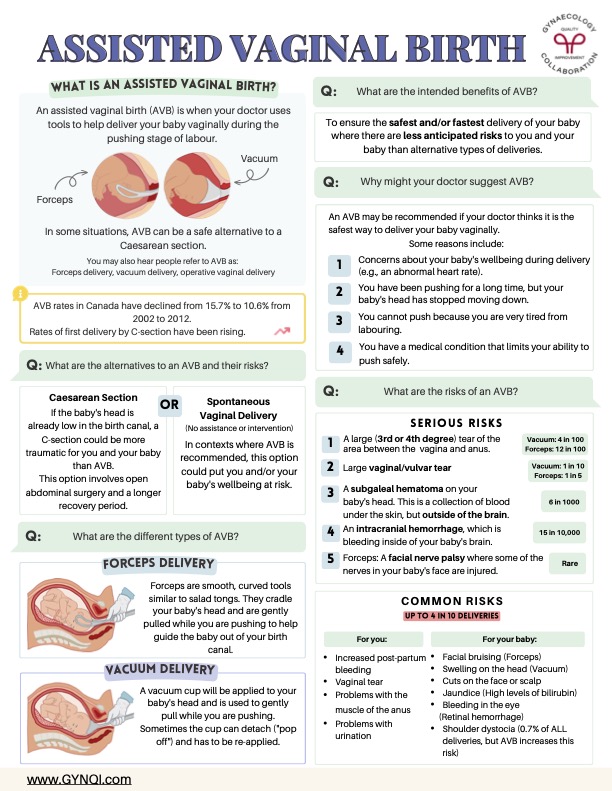
Getting to Know Assisted Vaginal Birth
An Assisted Vaginal Birth (AVB) is when your doctor uses tools to help deliver your baby vaginally during the pushing stage of labour. In a small number of births, AVB can be a safer alternative than a C-section or natural delivery.
You may also hear people refer to AVB as:
- Forceps delivery
- Vacuum delivery
- Operative vaginal delivery
AVB rates in Canada have declined from 15.7% to 10.6% from 2002 to 2012. However, the overall rate of first delivery by C-section is on the rise.
AVB Alternatives and Their Risks
Your obstetrician or doctor will only recommend AVB if they feel it is the safest choice for you and your baby at the time. The two main alternatives are a C-section or spontaneous vaginal delivery, both of which carry unique risks.
- C-Section: If the baby’s head is already low in the birth canal, a C-section could be more traumatic for you and your baby than AVB. This option involves open abdominal surgery and a longer recovery period.
- Spontaneous Vaginal Delivery: Some women are able to deliver without the need for assistance. In contexts where AVB is recommended, this option could put you and/or your baby’s well-being at risk.
Remember, the “perfect birth” is one where you and your baby are as healthy as possible when all is said and done. Things may not always go exactly as planned, but your care team will do everything they can to keep your risk for complications like these low.
What Are the Different Types of AVB?
Nearly all AVBs fall into one of two specific categories:
- Forceps Delivery: Forceps are smooth, curved tools similar to salad tongs. They cradle your baby’s head and are gently pulled while you are pushing to help guide the baby out of your birth canal.
- Vacuum Delivery: A vacuum cup will be applied to your baby’s head and is used to gently pull while you are pushing. Sometimes the cup can detach (“pop off”) and has to be re-applied.
It’s common for doctors and nurses to provide hands-on assistance to guide the baby out of the birth canal during vaginal deliveries. This can be helpful but isn’t the same as an AVB.
The Goal of An Assisted Birth
The core goal of any delivery, including AVB, is to preserve the health of the mother and baby to the greatest extent possible. AVB is usually recommended because it is less likely to expose you to unnecessary risks associated with an extremely long delivery or surgical procedures.
When Doctors Recommend AVB
An AVB may be recommended if your doctor thinks it is the safest way to deliver your baby vaginally. Some reasons include:
- Concerns about your baby’s well-being during delivery (e.g., an abnormal heart rate).
- You have been pushing for a long time, but your baby’s head has stopped moving down.
- You cannot push because you are very tired from labouring.
- You have a medical condition that limits your ability to push safely.
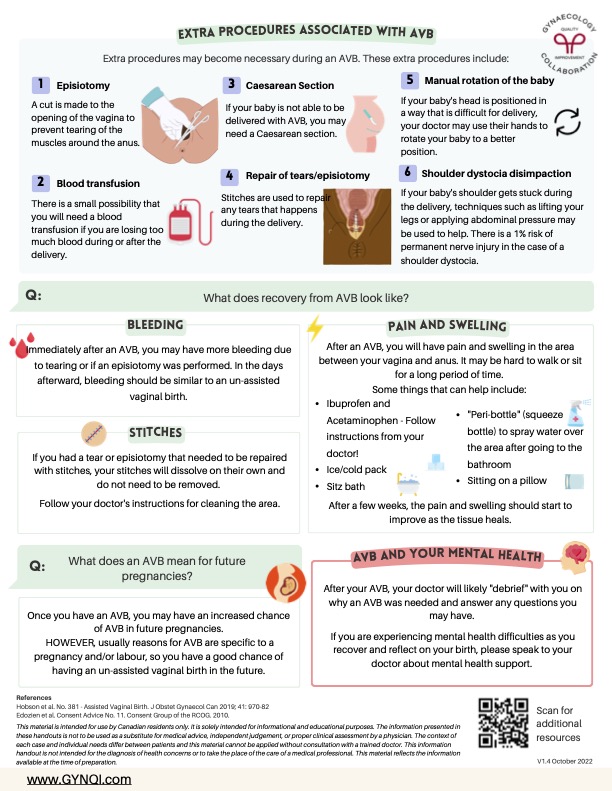
What Does an AVB Mean for Future Pregnancies?
Once you have an AVB, you have an increased chance of needing an AVB in future pregnancies. However, the reasons for AVB tend to be specific to an individual pregnancy and/or labour, so you have a good chance of having an unassisted vaginal birth in the future.
What Are the Risks of Assisted Vaginal Birth?
Most AVBs go smoothly without issue and result in a successful delivery with no further complications. Having an AVB can still raise the risk of certain complications or injuries for both you and your baby. The most serious potential outcomes include:
- A large (3rd or 4th degree) tear of the area between the vagina and anus (perineum). This occurs in about 4 in 100 vaccum births and 12 in 100 births with forceps.
- A large tear in the vaginal canal or vulva itself. This occurs in around 1 in 10 AVBs, including both vacuum and forceps delivery.
- A subgaleal hematoma on your baby’s head. This is a collection of blood under the skin, but outside of the brain. This occurs in 6 in 1000 AVBs.
- An intracranial hemorrhage, which is bleeding inside of your baby’s brain. This occurs in around 15 in 10,000 AVBs.
- A facial nerve palsy where some of the nerves in your baby’s face are injured. This is relatively rare and typically only occurs during AVBs with forceps.
Some of the risks associated with AVB are less serious, but are much more common. Issues like these occur in up to 4 in 10 assisted births:
For You:
- Increased post-partum bleeding
- Minor tears within the vagina or perineum
- Problems with the muscle of the anus
- Problems with urination
For Your Baby:
- Facial bruising (Forceps)
- Swelling on the head (Vacuum)
- Cuts on the face or scalp
- Jaundice (High levels of bilirubin)
- Bleeding in the eye (Retinal hemorrhage)
- Shoulder dystocia (0.7% of ALL deliveries, but AVB increases this risk)
Remember: having an increased risk for complications doesn’t automatically mean you or your baby will encounter any issues. Many assisted deliveries go as expected without any problems.
Extra Procedures
Sometimes, additional procedures are required during an AVB to ensure the safest possible delivery for you and your baby. For example:
- Episiotomy: A cut is made to the opening of the vagina to prevent tearing of the muscles around the anus.
- Blood Transfusion: There is a small possibility that you will need a blood transfusion if you are losing too much blood during or after the delivery.
- C-Section: If your baby is not able to be delivered with AVB, you may need an emergency c-section.
- Repair of Tears/Episiotomy: Stitches are used to repair any tears that happen during the delivery. Your doctor will numb your tissues with a freezing agent first.
- Manual Rotation of the Baby: If your baby’s head is positioned in a way that makes delivery challenging, your doctor may use their hands to rotate your baby.
- Shoulder Dystocia Disimpaction: If your baby’s shoulder gets stuck during delivery, techniques such as lifting your legs or applying abdominal pressure may help. There is a 1% risk of permanent nerve injury in the case of shoulder dystocia.
If you’re feeling anxious or afraid about having these procedures suddenly during your labour, speak to your doctor in advance. They can walk you through what each process looks like and how likely you are to need them.
Recovering From an AVB
Immediately after an AVB, you may have more bleeding due to tearing or if an episiotomy was performed. In the days afterward, bleeding should be similar to an unassisted vaginal birth.
If you had a tear or episiotomy that needed to be repaired with stitches, your stitches will dissolve on their own and do not need to be removed. Follow your doctor’s instructions for cleaning the area.
You may also experience pain and swelling in the area between your vagina and anus. It’s common for some people to find it difficult to walk or sit for a long period of time. To relieve pain and swelling, try:
- Ibuprofen and Acetaminophen: Follow instructions from your doctor.
- Ice/Cold Packs: Use an ice pack (or a frozen maxi pad) for 15 minutes every 2 hours.
- Sitz Baths: Soak your vagina in a bath with 2-3 inches of warm or cool water.
- A “Peri-bottle” (squeeze bottle): Spray water over the area after using the bathroom.
- Sitting on a Pillow: A regular cushion works, but ring pillows are even better.
After a few weeks, the pain and swelling should start to improve as the tissue heals. Let your doctor know right away if your symptoms worsen or the tissue starts to feel hot.
AVB and Your Mental Health
After your AVB, your doctor will likely “debrief” with you on why an AVB was needed and answer any questions you may have. You can ask for clarification on why you needed an assisted birth, whether they encountered any issues, and how AVB will affect your recovery.
If you are experiencing mental health difficulties as you recover and reflect on your birth, please speak to your doctor about mental health support. It’s completely normal to experience anxiety, disappointment, anger, or sadness after having an AVB—you aren’t alone!
Table of Contents
- Summary
- Introduction
- Getting to Know Assisted Vaginal Birth
- What Are the Different Types of AVB?
- The Goal of an Assisted Birth
- When Doctors Recommend AVB
- What does an AVB Mean for Future Pregnancies?
- What Are the Risks of an AVB?
- Extra Procedures
- Recovering From an AVB
- AVB and Your Mental Health
Summary:
- Labor and birth can be unpredictable. In a small percentage of births, doctors may need to step in and use forceps or a vacuum device to help deliver the baby—this is called an Assisted Vaginal Birth (AVB).
- Your doctor will only recommend an AVB if they are sure it is the best way to keep you and your baby safe while ensuring successful delivery. Asking questions about this process in advance can help you feel more in control.
- Forceps and vacuum deliveries do carry certain risks, although these risks are often lower than those associated with a c-section. You may also need additional procedures to facilitate AVB, such as an episiotomy or manual rotation of your baby.
- Having an AVB can slightly lengthen your recovery time after birth, and you may struggle with difficult emotions along the way. It’s completely normal to respond with anxiety, sadness, or even anger—your doctor can help you find ways to manage.
Assisted Vaginal Birth (AVB) typically involves using forceps or a vacuum suction device to gently guide the baby down the vaginal canal during pushing. This procedure can help labouring mothers deliver without the need for a Caesarean section (C-section), and may sometimes be the only safe option.
If you’re preparing to deliver your baby, or your doctor has informed you that you will likely need an AVB, you may be experiencing a mixture of feelings about it, including anxiety. Getting to know how an AVB happens and why can help you feel more confident and in control.
Getting to Know Assisted Vaginal Birth
An Assisted Vaginal Birth (AVB) is when your doctor uses tools to help deliver your baby vaginally during the pushing stage of labour. In a small number of births, AVB can be a safer alternative than a C-section or natural delivery.
You may also hear people refer to AVB as:
- Forceps delivery
- Vacuum delivery
- Operative vaginal delivery
AVB rates in Canada have declined from 15.7% to 10.6% from 2002 to 2012. However, the overall rate of first delivery by C-section is on the rise.
AVB Alternatives and Their Risks
Your obstetrician or doctor will only recommend AVB if they feel it is the safest choice for you and your baby at the time. The two main alternatives are a C-section or spontaneous vaginal delivery, both of which carry unique risks.
- C-Section: If the baby’s head is already low in the birth canal, a C-section could be more traumatic for you and your baby than AVB. This option involves open abdominal surgery and a longer recovery period.
- Spontaneous Vaginal Delivery: Some women are able to deliver without the need for assistance. In contexts where AVB is recommended, this option could put you and/or your baby’s well-being at risk.
Remember, the “perfect birth” is one where you and your baby are as healthy as possible when all is said and done. Things may not always go exactly as planned, but your care team will do everything they can to keep your risk for complications like these low.
What Are the Different Types of AVB?
Nearly all AVBs fall into one of two specific categories:
- Forceps Delivery: Forceps are smooth, curved tools similar to salad tongs. They cradle your baby’s head and are gently pulled while you are pushing to help guide the baby out of your birth canal.
- Vacuum Delivery: A vacuum cup will be applied to your baby’s head and is used to gently pull while you are pushing. Sometimes the cup can detach (“pop off”) and has to be re-applied.
It’s common for doctors and nurses to provide hands-on assistance to guide the baby out of the birth canal during vaginal deliveries. This can be helpful but isn’t the same as an AVB.
The Goal of An Assisted Birth
The core goal of any delivery, including AVB, is to preserve the health of the mother and baby to the greatest extent possible. AVB is usually recommended because it is less likely to expose you to unnecessary risks associated with an extremely long delivery or surgical procedures.
When Doctors Recommend AVB
An AVB may be recommended if your doctor thinks it is the safest way to deliver your baby vaginally. Some reasons include:
- Concerns about your baby’s well-being during delivery (e.g., an abnormal heart rate).
- You have been pushing for a long time, but your baby’s head has stopped moving down.
- You cannot push because you are very tired from labouring.
- You have a medical condition that limits your ability to push safely.
What Does an AVB Mean for Future Pregnancies?
Once you have an AVB, you have an increased chance of needing an AVB in future pregnancies. However, the reasons for AVB tend to be specific to an individual pregnancy and/or labour, so you have a good chance of having an unassisted vaginal birth in the future.
What Are the Risks of Assisted Vaginal Birth?
Most AVBs go smoothly without issue and result in a successful delivery with no further complications. Having an AVB can still raise the risk of certain complications or injuries for both you and your baby. The most serious potential outcomes include:
- A large (3rd or 4th degree) tear of the area between the vagina and anus (perineum). This occurs in about 4 in 100 vaccum births and 12 in 100 births with forceps.
- A large tear in the vaginal canal or vulva itself. This occurs in around 1 in 10 AVBs, including both vacuum and forceps delivery.
- A subgaleal hematoma on your baby’s head. This is a collection of blood under the skin, but outside of the brain. This occurs in 6 in 1000 AVBs.
- An intracranial hemorrhage, which is bleeding inside of your baby’s brain. This occurs in around 15 in 10,000 AVBs.
- A facial nerve palsy where some of the nerves in your baby’s face are injured. This is relatively rare and typically only occurs during AVBs with forceps.
Some of the risks associated with AVB are less serious, but are much more common. Issues like these occur in up to 4 in 10 assisted births:
For You:
- Increased post-partum bleeding
- Minor tears within the vagina or perineum
- Problems with the muscle of the anus
- Problems with urination
For Your Baby:
- Facial bruising (Forceps)
- Swelling on the head (Vacuum)
- Cuts on the face or scalp
- Jaundice (High levels of bilirubin)
- Bleeding in the eye (Retinal hemorrhage)
- Shoulder dystocia (0.7% of ALL deliveries, but AVB increases this risk)
Remember: having an increased risk for complications doesn’t automatically mean you or your baby will encounter any issues. Many assisted deliveries go as expected without any problems.
Extra Procedures
Sometimes, additional procedures are required during an AVB to ensure the safest possible delivery for you and your baby. For example:
- Episiotomy: A cut is made to the opening of the vagina to prevent tearing of the muscles around the anus.
- Blood Transfusion: There is a small possibility that you will need a blood transfusion if you are losing too much blood during or after the delivery.
- C-Section: If your baby is not able to be delivered with AVB, you may need an emergency c-section.
- Repair of Tears/Episiotomy: Stitches are used to repair any tears that happen during the delivery. Your doctor will numb your tissues with a freezing agent first.
- Manual Rotation of the Baby: If your baby’s head is positioned in a way that makes delivery challenging, your doctor may use their hands to rotate your baby.
- Shoulder Dystocia Disimpaction: If your baby’s shoulder gets stuck during delivery, techniques such as lifting your legs or applying abdominal pressure may help. There is a 1% risk of permanent nerve injury in the case of shoulder dystocia.
If you’re feeling anxious or afraid about having these procedures suddenly during your labour, speak to your doctor in advance. They can walk you through what each process looks like and how likely you are to need them.
Recovering From an AVB
Immediately after an AVB, you may have more bleeding due to tearing or if an episiotomy was performed. In the days afterward, bleeding should be similar to an unassisted vaginal birth.
If you had a tear or episiotomy that needed to be repaired with stitches, your stitches will dissolve on their own and do not need to be removed. Follow your doctor’s instructions for cleaning the area.
You may also experience pain and swelling in the area between your vagina and anus. It’s common for some people to find it difficult to walk or sit for a long period of time. To relieve pain and swelling, try:
- Ibuprofen and Acetaminophen: Follow instructions from your doctor.
- Ice/Cold Packs: Use an ice pack (or a frozen maxi pad) for 15 minutes every 2 hours.
- Sitz Baths: Soak your vagina in a bath with 2-3 inches of warm or cool water.
- A “Peri-bottle” (squeeze bottle): Spray water over the area after using the bathroom.
- Sitting on a Pillow: A regular cushion works, but ring pillows are even better.
After a few weeks, the pain and swelling should start to improve as the tissue heals. Let your doctor know right away if your symptoms worsen or the tissue starts to feel hot.
AVB and Your Mental Health
After your AVB, your doctor will likely “debrief” with you on why an AVB was needed and answer any questions you may have. You can ask for clarification on why you needed an assisted birth, whether they encountered any issues, and how AVB will affect your recovery.
If you are experiencing mental health difficulties as you recover and reflect on your birth, please speak to your doctor about mental health support. It’s completely normal to experience anxiety, disappointment, anger, or sadness after having an AVB—you aren’t alone!



