Table of Contents
- Summary
- What is Endometrial Cancer?
- Risk Factors for Endometrial Cancer
- Type I Endometrial Cancer
- Type II Endometrial Cancer
- Symptoms of Endometrial Cancer
- Diagnosing Endometrial Cancer
- Bloodwork Investigations
- Imaging
- Endometrial Biopsies
- Empowering Yourself in Your Healthcare Decisions
Summary:
- Endometrial cancer develops in the lining of the uterus (endometrium) and is the most common gynaecologic cancer in North America, with a lifetime risk of 2.6%. Its likelihood can be influenced by various risk factors.
- There are two main types of endometrial cancer: Type I, which is hormone-related and accounts for up to 80% of cases, and Type II, which is less common and not associated with hormones. Risk factors for Type I include obesity, high blood pressure, and never having been pregnant, while Type II is more prevalent in older adults and may involve genetic mutations.
- The primary symptom of endometrial cancer is abnormal bleeding, experienced by up to 95% of patients. Recognizing this symptom early, especially in postmenopausal women, is crucial for effective management and timely intervention.
- Diagnosis of endometrial cancer involves several approaches, including imaging techniques like pelvic ultrasounds and sonohysterograms, as well as endometrial biopsies to assess the uterine lining directly.
Endometrial cancer, the most common gynaecologic cancer in North America, affects the lining of the uterus, called the endometrium. There are two main types, each with distinct risk factors–Type I is often hormone-related and linked to excess estrogen, obesity, and other health conditions, while Type II is typically unrelated to hormones and includes rare and aggressive forms.
Early symptoms, primarily abnormal bleeding, can guide timely diagnosis, which involves imaging, sonohysterograms, and endometrial biopsies. Identifying risk factors and symptoms is crucial for early intervention, which significantly improves outcomes.
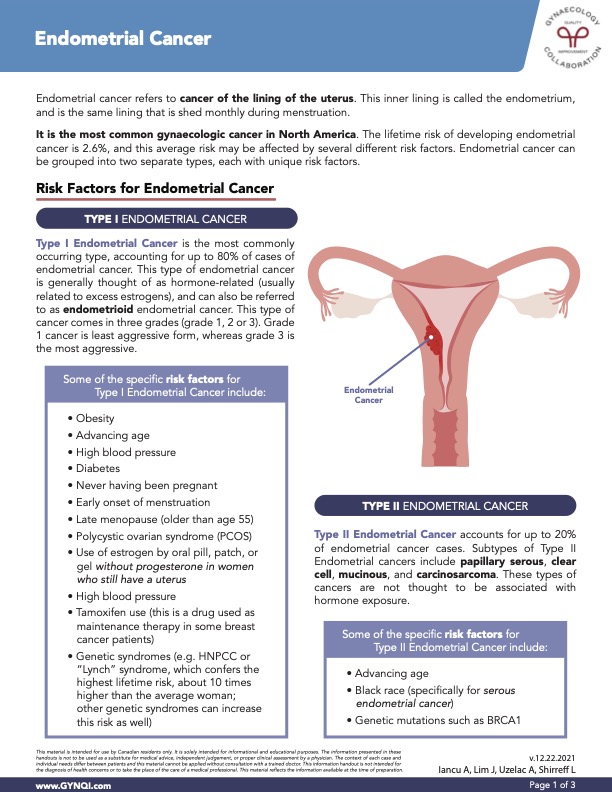
What is Endometrial Cancer?
Endometrial cancer is a type of cancer that develops in the lining of the uterus, known as the endometrium—the same tissue shed each month during menstruation.
It is the most common gynecologic cancer in North America, with a lifetime risk of 2.6%, though various risk factors can influence this likelihood.
Risk Factors for Endometrial Cancer
Endometrial cancer can be grouped into two separate types, each with unique risk factors.
Type I Endometrial Cancer
Type I Endometrial Cancer is the most commonly occurring type, accounting for up to 80% of cases of endometrial cancer. This type of endometrial cancer is generally thought of as hormone-related and usually related to excess estrogens. It can also be referred to as endometrioid endometrial cancer.
This type of cancer comes in three grades (grade one, two, or three). Grade One cancer is the least aggressive form, whereas Grade Three is the most aggressive.
Some of the specific risk factors for Type I Endometrial Cancer include:
- Obesity
- Advancing age
- High blood pressure
- Diabetes
- Never having been pregnant
- Early onset of menstruation
- Late menopause (older than age 55)
- Polycystic ovarian syndrome (PCOS)
- Use of estrogen by oral pill, patch, or gel without progesterone in those who still have a uterus
- High blood pressure
- Tamoxifen use (a maintenance therapy drug used in some breast cancer patients)
- Genetic syndromes (e.g. HNPCC or “Lynch” syndrome, resulting in a lifetime risk up to 10 times higher than average)
Type II Endometrial Cancer
Type II Endometrial Cancer accounts for up to 20% of endometrial cancer cases. Subtypes of Type II Endometrial cancers include papillary serous, clear cell, mucinous, and carcinosarcoma. These types of cancers are not thought to be associated with hormone exposure.
Some of the specific risk factors for Type II Endometrial Cancer include:
- Advancing age
- Black race (specifically for serous endometrial cancer)
- Genetic mutations such as BRCA1
Symptoms of Endometrial Cancer
Identifying symptoms of endometrial cancer early is key for effective management and timely care.
Abnormal bleeding is the most common symptom of endometrial cancer and occurs in up to 95% of patients.
- Premenopausal: In people who are still menstruating, this may manifest as increased flow or frequency of periods or bleeding between periods.
- Postmenopausal: In people who have experienced menopause (over 12 months since their last period), abnormal bleeding is postmenopausal bleeding, and can point to uterine cancer in 10% of cases.
Around 5% of cases will not have abnormal bleeding or discharge, and endometrial cancers may be alternatively diagnosed through other investigations including:
- Abnormal Pap test
- Abnormal appearance of endometrium, or uterine lining, on imaging
- Abnormal pathology at the time of hysterectomy or dilation and curettage (D&C) for unrelated reasons
Diagnosing Endometrial Cancer
To diagnose endometrial cancer, healthcare providers use a range of methods to ensure accuracy and early intervention.
Bloodwork Investigations
Endometrial cancer cannot be diagnosed using bloodwork.
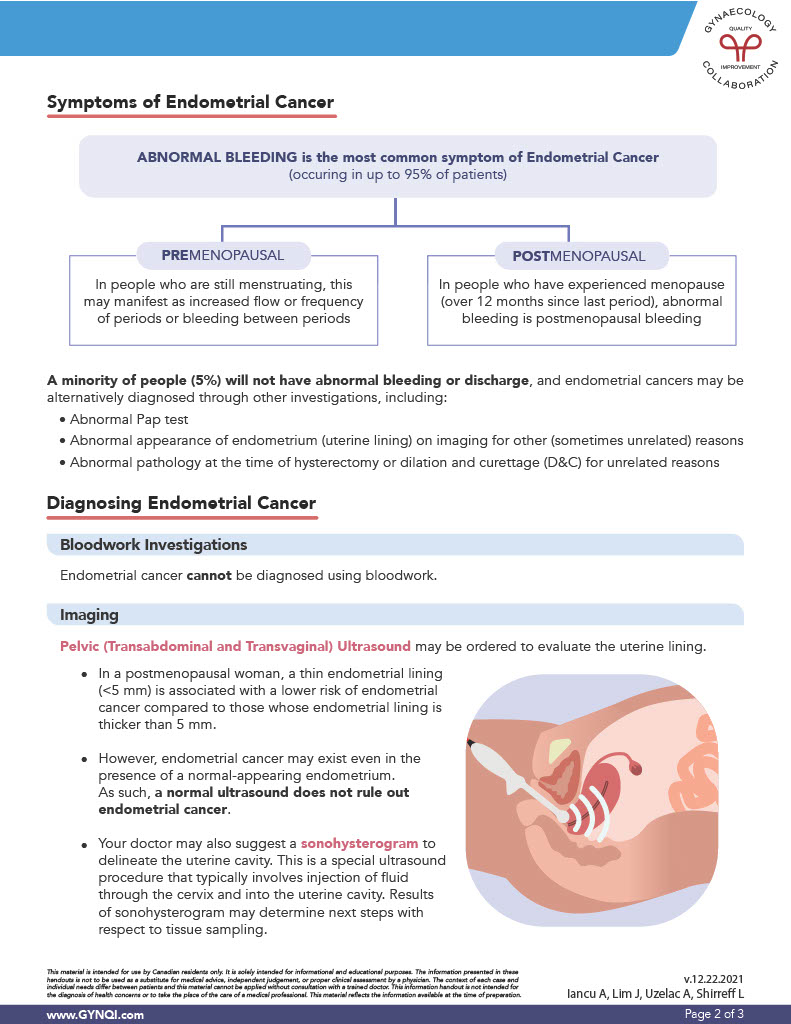
Imaging
A pelvic ultrasound, including both transabdominal and transvaginal approaches, may be ordered to assess the uterine lining.
In a postmenopausal woman, a thin endometrial lining (<5 mm) is associated with a lower risk of endometrial cancer compared to those whose endometrial lining is thicker than 5 mm. However, endometrial cancer may exist even in the presence of a normal-appearing endometrium.
Your doctor may also recommend a sonohysterogram to get a clear view of the inside of the uterus. This is a special ultrasound procedure that typically involves the injection of fluid through the cervix and into the uterine cavity. The results of sonohysterogram may determine the next steps with respect to tissue sampling.
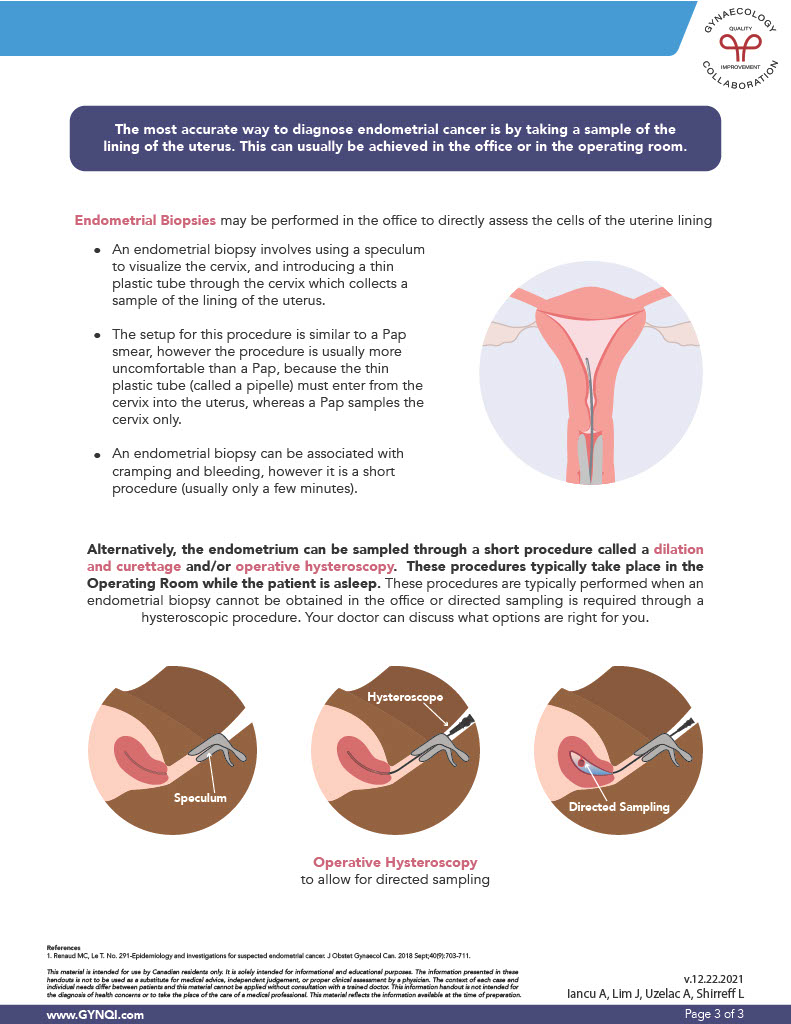
Endometrial Biopsies
Endometrial biopsies may be performed in the office to directly assess the cells of the uterine lining. An endometrial biopsy involves using a speculum to visualize the cervix and introducing a thin plastic tube through the cervix which collects a sample of the lining of the uterus.
The setup for this procedure is similar to a Pap smear but can be more uncomfortable than a Pap because the pipelle (the thin plastic tube) must enter from the cervix into the uterus, whereas a Pap samples the cervix only.
An endometrial biopsy can be associated with cramping and bleeding, however, it is a short procedure and usually only takes a few minutes.
Empowering Yourself in Your Healthcare Decisions
Cancer can be a scary word. Being armed with knowledge helps you notice the symptoms of endometrial cancer so you can take action, giving you the best chances at early intervention. If you have abnormal bleeding, and have certain risk factors such as high blood pressure and polycystic ovarian syndrome, speak to your medical care team. They can offer further evaluation, conduct necessary tests, and guide you through the next steps.
Remember, early detection is key to improving outcomes, and your health is worth advocating for.



