Table of Contents
- Summary
- What is Endometrial Hyperplasia?
- Types of Endometrial Hyperplasia
- Endometrial Hyperplasia with Atypia
- Endometrial Hyperplasia Without Atypia
- Diagnosis of Endometrial Hyperplasia
- Treatment of Endometrial Hyperplasia
- Treatment for Endometrial Hyperplasia with Atypia
- Treatment for Endometrial Hyperplasia Without Atypia
- Taking Charge of Your Health and Wellness
- Frequently Asked Questions
Summary:
- Endometrial hyperplasia is the abnormal thickening of the uterine lining, characterized by cells that grow in a crowded, disorganized way.
- This condition can be categorized as “with atypia”, which carries a higher risk of progressing to endometrial cancer, or “without atypia”, which has a significantly lower risk.
- Endometrial hyperplasia is typically diagnosed through an endometrial biopsy, which may be performed in an office setting or under anesthesia for patient comfort.
- Management varies based on the type of hyperplasia, with surgical options recommended for “with atypia” cases, while “without atypia” cases may be treated with hormonal therapy.
Endometrial hyperplasia is the abnormal thickening of the uterine lining, where cells grow in a crowded and/or disorganized manner. While the endometrium normally thickens and sheds during menstrual cycles, it should remain thin and bleed-free after menopause. If untreated, this condition can lead to endometrial cancer. Endometrial hyperplasia can manifest as “with atypia”, which has a higher cancer risk, or “without atypia”, which poses a lower risk. Understanding these variations is essential for effective management and treatment of the condition.
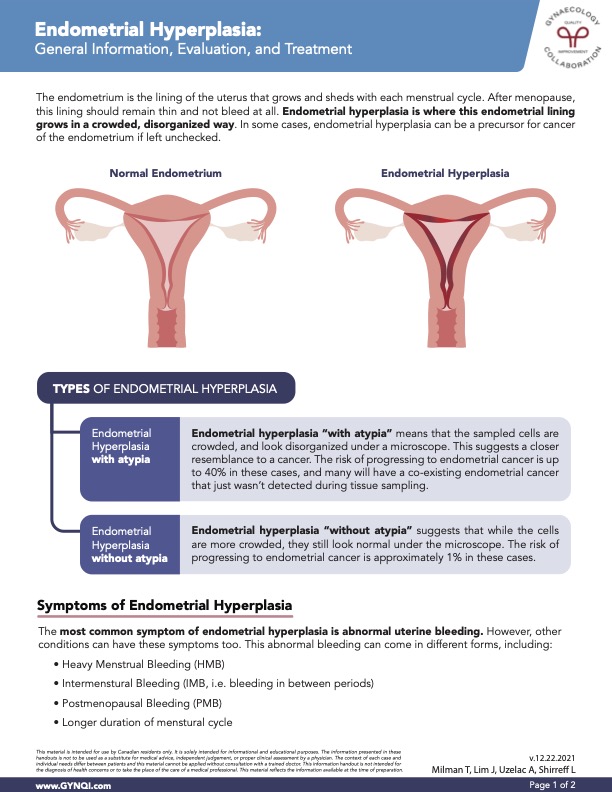
What is Endometrial Hyperplasia?
Endometrial hyperplasia is where the endometrial lining grows in a crowded, disorganized way. The endometrium is the lining of the uterus that grows and sheds with each menstrual cycle.
Endometrial hyperplasia primarily affects women in their 50s and 60s who have experienced menopause, but it can also occur in those undergoing perimenopause, characterized by irregular menstrual periods.
After menopause, this lining should remain thin and not bleed at all. In some cases, endometrial hyperplasia can be a precursor for cancer of the endometrium if left unchecked.

Types of Endometrial Hyperplasia
Endometrial hyperplasia, a condition marked by the thickening of the uterine lining, can manifest in various forms, each with differing risks and implications for future health.
Endometrial Hyperplasia with Atypia
Endometrial hyperplasia “with atypia” means that the sampled cells are crowded and look disorganized under a microscope. This suggests a closer resemblance to cancer. The risk of progressing to endometrial cancer is up to 40% in these cases, and many will have a co-existing endometrial cancer that wasn’t detected during tissue sampling.
Endometrial Hyperplasia Without Atypia
Endometrial hyperplasia “without atypia” suggests that while the cells are more crowded, they still look normal under the microscope. The risk of progressing to endometrial cancer is approximately 1% in these cases.
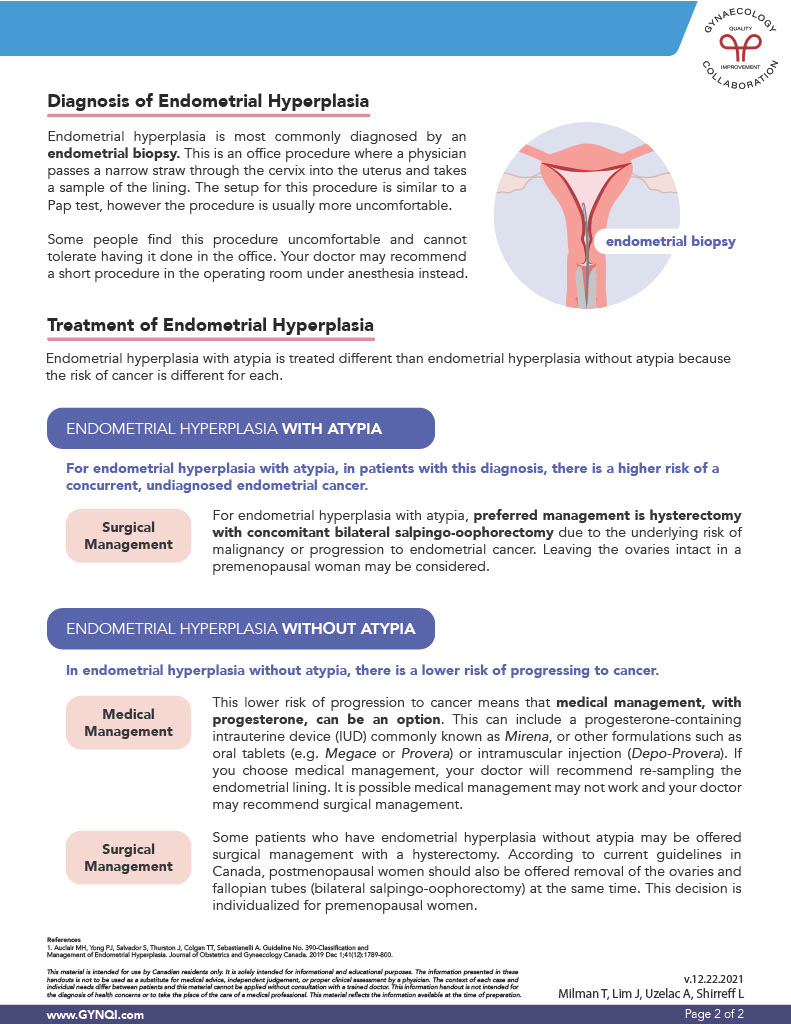
Diagnosis of Endometrial Hyperplasia
Endometrial hyperplasia is most commonly diagnosed by an endometrial biopsy. This is an office procedure where a physician passes a narrow straw through the cervix into the uterus and takes a sample of the lining. The setup for this procedure is similar to a Pap test, however the procedure can be more uncomfortable.
For those who find the procedure uncomfortable or difficult to tolerate in the office, your doctor may recommend a brief procedure in the operating room under anesthesia as an alternative.

Treatment of Endometrial Hyperplasia
The treatment approach for endometrial hyperplasia varies, as the risk of developing cancer differs between hyperplasia with atypia and without atypia.
Treatment for Endometrial Hyperplasia with Atypia
In cases of endometrial hyperplasia with atypia, patients face a higher risk of having an undiagnosed, concurrent endometrial cancer.
Surgical Management: For endometrial hyperplasia with atypia, the recommended treatment is usually a hysterectomy with the removal of both ovaries and fallopian tubes (concomitant bilateral salpingo-oophorectomy), as there’s a risk of cancer or progression to endometrial cancer. However, in premenopausal women, leaving the ovaries intact may be an option.
Treatment for Endometrial Hyperplasia Without Atypia
In endometrial hyperplasia without atypia, there is a lower risk of progressing to cancer.
Medical Management: This lower risk of progression to cancer means that medical management, with progesterone, can be an option. This can include:
- An intrauterine device (IUD), commonly known as Mirena
- Oral tablets (e.g. Megace or Provera)
- Intramuscular injection (Depo-Provera)
If you choose medical management, your doctor will recommend re-sampling the endometrial lining. It is possible medical management may not work and your doctor may recommend surgical management.
Surgical Management: Some patients who have endometrial hyperplasia without atypia may be offered surgical management with a hysterectomy.
According to current guidelines in Canada, postmenopausal women should also be offered removal of the ovaries and fallopian tubes (bilateral salpingo-oophorectomy) at the same time. This decision is individualized for premenopausal women.
Taking Charge of Your Health and Wellness
The approach to treating endometrial hyperplasia depends on whether atypia is present, with more aggressive options like hysterectomy being recommended for higher-risk cases, and medical management with progesterone more appropriate for lower-risk patients without atypia. Individual treatment plans should be tailored to each patient’s unique circumstances, including age and cancer risk.
Empowering yourself in your health journey allows you to navigate challenges with confidence, armed with the information and resources you need to be your best advocate.
Frequently Asked Questions About Endometrial Hyperplasia
What is endometrial hyperplasia, and what causes it?
Changing hormone levels in the body can make endometrial hyperplasia more common during perimenopause and menopause. Irregular ovulation sometimes leads to prolonged exposure to estrogen and less exposure to progesterone, which makes hyperplasia more common.
In postmenopause, any abnormal thickening of the uterine lining is particularly concerning, as it’s no longer influenced by the menstrual cycle. Postmenopausal bleeding or spotting is one of the key warning signs of endometrial hyperplasia and should always be evaluated by a doctor.
What symptoms of endometrial hyperplasia should I watch for?
The most common symptoms include heavy or prolonged periods, spotting between periods, or bleeding after menopause. it’s important to talk to your doctor if you notice changes like these, even if they’re mild or don’t interfere with your life. Early diagnosis can help!
Can lifestyle changes help prevent or manage endometrial hyperplasia?
Yes. Maintaining a healthy weight and managing secondary conditions like Polycystic Ovarian Syndrome (PCOS) can help lower your risk for hyperplasia.
If you’re on hormone replacement therapy for menopause, make sure it includes progesterone unless your doctor says otherwise. Regular checkups can also catch changes early, which is the best way to prevent hyperplasia from progressing.
Does endometrial hyperplasia ever go away on its own?
In most cases, endometrial hyperplasia won’t resolve without treatment. Hormonal therapies, like oral progestins, can help thin the lining of the uterus and prevent the condition from progressing. Certain types of hyperplasia can progress to more serious conditions, which is why it’s important to address any symptoms with your doctor right away.
How often should I see my doctor if I have endometrial hyperplasia?
Your follow-up schedule will depend on the type of hyperplasia you have, the severity of your condition, and your treatment plan. If you’re on hormonal therapy, your doctor may want to connect at least once every three to six months so they can monitor your progress.
For atypical hyperplasia, more frequent evaluations or imaging may be necessary. Ask your doctor for more information if you aren’t sure which schedule is best.



