Endometrial Polyps: General Information
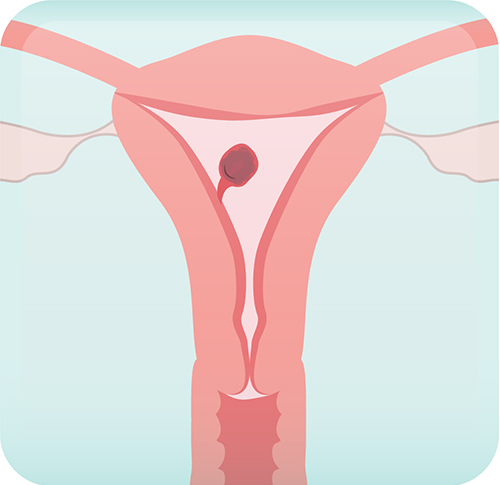
Endometrial polyps represent overgrowths of endometrial tissue (i.e. the inner uterine lining) that protrude
into the uterine cavity. Polyps can be thought of as “skin tags” of the uterus.
- Endometrial polyps are common and may occur in up to 35% of women. However, this proportion may be underestimated. Many people with polyps don’t have symptoms, so they go undiagnosed.
- Endometrial polyps are sometimes incidentially diagnosed at the time of pelvic ultrasounds being completed for another reason.
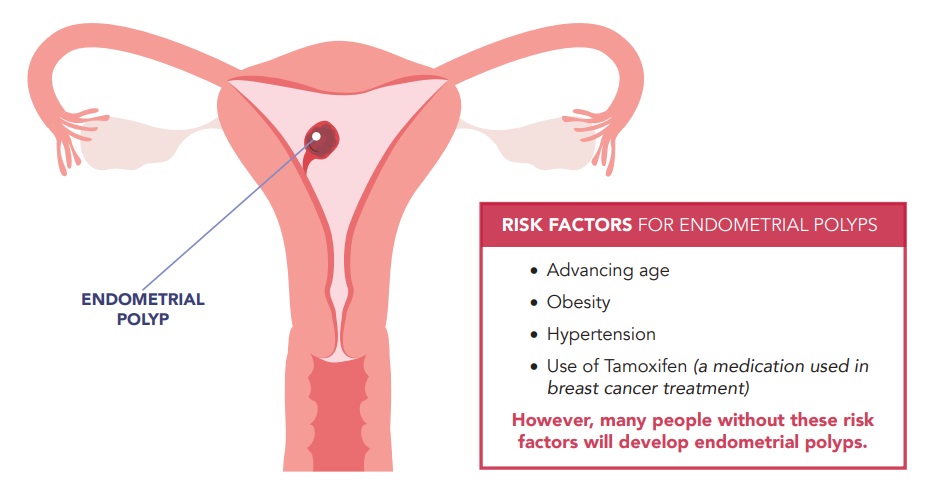
The majority (90%) of endometrial polyps are benign. However, some endometrial polyps may contain precancerous or cancerous cells. The risk of cancer in endometrial polyps ranges between 0 – 12% depending on the patient population. The risk of a polyp being cancer goes up with increasing patient age, presence of symptoms, increasing polyp size, and history of Tamoxifen use.
Symptoms of Endometrial Polyps
Most endometrial polyps are not associated with symptoms. Endometrial polyps are not likely to be associated with pelvic pain, pressure, bloating, or bowel/bladder symptoms.
- Of those who are symptomatic, the most common symptom is abnormal vaginal bleeding
- Other symptoms include difficulty getting pregnant in women of reproductive age
Endometrial Polyps: Evaluation
Endometrial polyps cannot be diagnosed with bloodwork and typically require imaging as the first step to
diagnosis. Most commonly, endometrial polyps are diagnosed as part of the work-up for other reasons or
symptoms, such as abnormal vaginal bleeding or infertility.
1. Transvaginal Ultrasound
Your physician will usually order a pelvic and/or transvaginal ultrasound (TVUS) as the first type of imaging for suspected endometrial polyps.
A pelvic ultrasound uses an external probe on your lower abdomen to provide images of your pelvic structures. A transvaginal ultrasound may be completed at the same time, with your consent. In a TVUS, a probe is inserted into the vagina to better delineate the female reproductive organs.
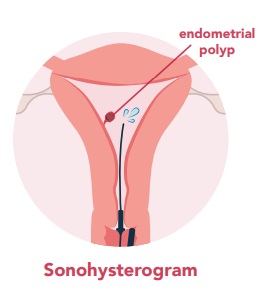
2. Sonohysterogram
A sonohysterogram may also be suggested to assess the cavity of the uterus and determine if any submucosal fibroids are present that indent into the uterine cavity.
This is a procedure that typically involves insertion of a speculum followed
by injection of fluid through the cervix and into the uterine cavity. An
ultrasound is completed at the same time, which provides a more detailed assessment of your uterus. Specifically, this test will tell your doctor about whether there are any structures in the cavity of your uterus such as endometrial polyps and how big they are.
...a quick note on tissue biopsies
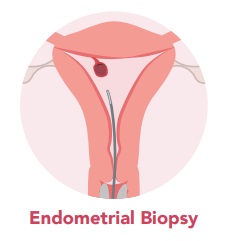
Depending on factors relating to the risk that a polyp may
contain precancerous or cancerous cells (e.g. age, polyp size), an endometrial biopsy may be suggested. This is a short office procedure where the inner lining of the uterus is sampled with a small pipelle inserted through the cervix. This is a blind procedure that may or may not capture the polyp itself.
Typically, endometrial polyps are removed under direct visualization (e.g. hysteroscopic polypectomy). The tissue obtained will be reviewed by a pathologist trained to assess for the presence of precancerous or cancerous cells.
Endometrial Polyps: Treatment
Management of endometrial polyps depends on the specific clinical situation. Bothersome symptoms, fertility concerns, or cancer risk can affect treatment decisions when it comes to endometrial polyps.
Management options fit into two categories: expectant management or surgical removal. There are no medications that are currently recommended for the treatment of endometrial polyps.
Expectant Management of Polyps
Where appropriate (e.g. asymptomatic premenopausal women), endometrial polyps can simply be left alone.
Some studies suggest that up to 25% of these polyps, especially if small (<10 mm), may regress on their own
or slough off with a period.
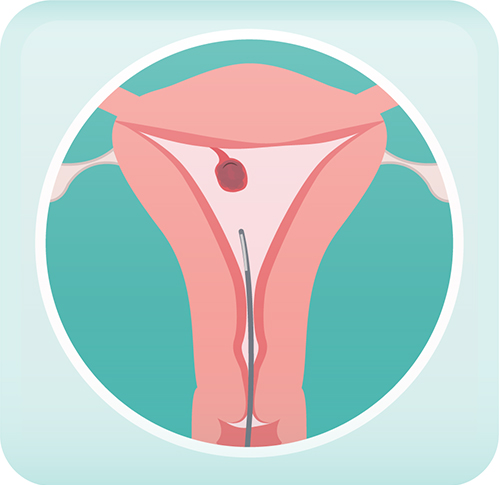
Surgical Management of Polyps — the procedure is called a hysteroscopic polypectomy
This surgery is typically performed by introducing a camera into the uterine cavity through the vagina with an
instrument called a hysteroscope. The polyp is then removed via a very thin instrument introduced through
the hysteroscope. It does not involve any incisions into your abdomen and is considered minimally invasive.
Most patients are able to be discharged home a few hours after surgery and do not require an overnight stay.
Premenopausal
In premenopausal women with fertility concerns or with abnormal bleeding, investigations may reveal endometrial polyps. In such cases, surgical removal is often recommended.
Postmenopausal
Postmenopausal women diagnosed with endometrial polyps often require surgical removal, especially if they are causing symptoms. Other factors physicians may consider when determining whether a postmenopausal patient requires a hysteroscopic polypectomy include the size of the polyp(s) and patient age. These factors relate to the risk that a polyp may contain precancerous or cancerous cells.
Generally, a hysterectomy (removal of the uterus) is not required to treat polyps, unless there is evidence of endometrial cancer or, in most cases, hyperplasia (precancerous cells).
In order to determine whether expectant management or surgery is right for you, many factors, as noted above, must be considered. Please speak to your physician about your treatment options and their recommendations before making a decision.