Complete Guide to Endometriosis
Endometriosis is a chronic condition that affects 1 in 10 people with ovaries. It can cause pain, infertility and ovarian cysts. For general information on endometriosis, access our patient handout.
We are pleased to provide resources below that were created by endometriosis specialists. Our aim is to provide you with trusted information on the treatments for endometriosis.
What is Endometriosis?
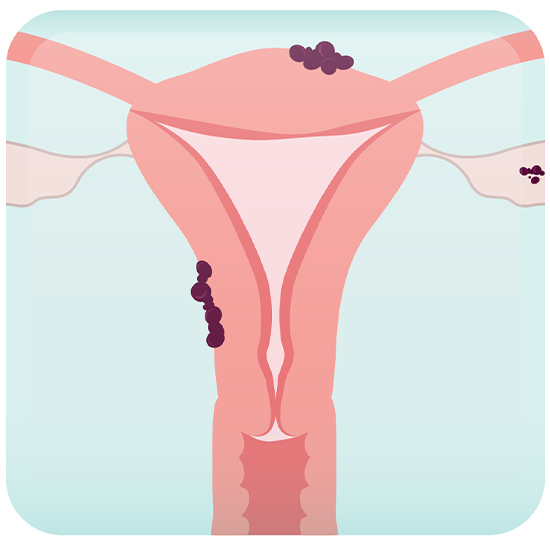
Endometriosis occurs when tissue that resembles the inner lining of the uterus (i.e. endometrium) is found outside of the uterus.
Estrogen plays an important role in endometriosis growth. During each menstrual cycle, there is an increase in estrogen within the body. Implants of endometriosis may swell, grow and bleed, just like the endometrial lining inside the uterus. This swelling and bleeding at endometriosis sites causes pain through local inflammation, new blood vessel formation (angiogenesis), and nerve cell formation (neurogenesis).
The symptoms of endometriosis vary from person to person. Endometriosis implants can be found on ovaries, causing cysts called endometriomas (also called chocolate cysts). They can also be found on the uterus, vagina, bowels, urinary bladder, pelvic muscles, and nerves. Various symptoms can be associated with endometriosis and sometimes depend on the location of implants in the pelvis or abdomen.
Symptoms of endometriosis can include:
- Dysmenorrhea (painful periods)
- Dyspareunia (painful intercourse)
- Dyschezia (painful bowel movements)
- Dysuria (painful or frequent urination)
- Infertility
- Chronic pelvic pain
Endometriosis can be challenging to diagnose and manage. The most common age at diagnosis of endometriosis is between ages 35 and 44 years.
- Frequently, endometriosis is diagnosed based on a combination of presenting symptoms, physical exam findings, and imaging. There is no single test or imaging modality that can diagnose endometriosis definitively.
- Ultrasound will sometimes show ovarian cysts (endometriomas), scarring or more advanced deeply infiltrating endometriosis. MRI can sometimes be a second-line imaging modality that can also be helpful in diagnosing.
- Surgery is NO LONGER a first-line method to diagnose endometriosis.
Medical therapies are the cornerstone of endometriosis management and have been recommended as first-line treatments. Common treatments include the use of:
- Birth Control Pills
- Oral Progestin
- Progestin IUD
- GnRH Antagonist
- GnRH Agonist
Endometriosis is a chronic condition that has a very high chance of coming back. Even after surgery, medical therapies are recommended to prevent disease recurrence in those not trying to get pregnant. There is no one-size-fits-all solution.
Commonly, a laparoscopy is performed with the goal of resecting any endometriosis implants. Surgical management is typically suggested after medical options are trialed and found to be ineffective at controlling symptoms. Other times surgery is recommended:
- To help patients with infertility and endometriosis in certain circumstances
- Remove large endometriomas (>4cm)
- In patients with deeply infiltrating endometriosis penetrating the bowel or urinary system
Endometriosis is a chronic condition that can come back after surgery. Discuss ways to suppress the disease with medicine after surgery to prevent recurrence.
Medical Treatment Options

Birth Control Pills
- 20-50% reduction in menstrual bleeding
- CHC use associated with reduction in pain during period (dysmenorrhea) & pre-menstrual symptoms
- CHCs can be taken continuously so people with endometriosis don’t get a period
Yes
- CHCs have no impact on future fertility
Breast tenderness, mood changes, fluid retention, and breakthrough bleeding
Oral Progestins (Access handouts here)
Oral Progestins
- Pills taken by mouth
- Stop growth of endometriosis tissue
- Can shrink ovarian cysts of endometriosis
- Can stop menstruation
- Effective in decreasing pain
NO
- use condoms or non-hormonal intrauterine device for contraception
Irregular or unscheduled vaginal bleeding is common for first 3-6 months, headache, breast tenderness, occasional hot flashes
Progestin IUD
- 70-97% reduction in menstrual bleeding
- Absence of menstruation (amenorrhea) experienced by 20-80% of patients after 1 year of use
- LNG-IUD use associated with reduction in menstrual cramps and/or pain during period
Yes
- LNG-IUD has no impact on future fertility
Irregular bleeding during first 6 months, breast tenderness, acne, cramping, headaches
GnRH Agonists (Access handout here)
GnRH Agonist
- Improves pain from endometriosis
- Stops heavy periods and improves your body’s iron stores
- Shrinks fibroids and ovarian cysts
No
- use condoms or non-hormonal intrauterine device for contraception
Menopause symptoms (eg. hot flashes, night sweats, vaginal dryness, sleep disturbance) can be decreased by taking add-back hormones
Frequently Asked Questions Endometriosis
Endometriosis cannot be cured, however there are medications to address the symptoms, mainly pain. Not all patients can take every medication. Your doctor will determine whether you are a suitable candidate.
Yes, endometriosis can affect fertility. However, not all women with endometriosis experience infertility.
After discussion with your healthcare provider, the medical therapy you choose will depend on:
- Your Symptoms
- Your Need for Contraception
- Other Conditions you may have (e.g., fibroids, adenomyosis)
- Your Medical History
- Your Side-Effect Profile
- Costs
Shared decision-making is most important, so be sure to engage your healthcare provider in these discussions.
The exact cause of endometriosis is not fully known, but potential factors include retrograde menstruation (when menstrual blood flows backward into the pelvic cavity), hormonal imbalances, immune system disorders, and genetic predisposition.