Table of Contents
- Summary
- Introduction
- Evaluating for Fibroids
- History
- Physical Examination
- Abdominal Exam
- Pelvic Exam
- Imaging
- Further Investigations
- Endometrial Biopsy
- Exploratory Surgery
- Bloodwork
- Creatinine
- Should All Fibroids Be Treated?
Summary:
- Fibroids are benign (non-cancerous) growths that sometimes develop on or inside of the uterus in people of childbearing age. They may occur silently or cause debilitating symptoms like pain, heavy bleeding, and fertility problems.
- Getting evaluated for fibroids is important, regardless of your symptoms. While they rarely become malignant, having one growth makes you more likely to develop additional growths over time. They can eventually lead to infertility or anemia.
- To diagnose you with fibroids, your doctor may take a careful history, do a physical exam, or order imaging and bloodwork. Each of these types of tests can provide important clues to the size, location, and shape of fibroids.
- Not all fibroids require intervention. In some cases, your doctor may recommend a wait-and-see approach. This is especially true if you are nearing menopause, as your risk of developing fibroids drops sharply after your periods stop.
Fibroids are benign growths (tumors) that develop on or within the uterus, typically in women of childbearing age. Your doctor may suspect you have fibroids based on the symptoms you report, such as heavy menstrual bleeding, pelvic pressure, or pain. Alternatively, they may notice signs of a fibroid during a routine pelvic exam or during unrelated pelvic imaging.
If you have reason to suspect you have fibroids, tell your provider right away. He or she can help you navigate the process of evaluation and get the treatment you need.
Why Get Evaluated for Fibroids?
In almost all cases, fibroids are non-cancerous. They are also highly unlikely to become malignant over time, even if you do nothing to treat them, and don’t raise your risk for developing other types of cancer. In fact, only 1 in 1000 fibroids go on to become malignant (called a leiomyosarcoma).
But just because fibroids are benign doesn’t mean they can’t cause issues. For some women, they can cause painful or challenging symptoms like heavy menstrual bleeding, chronic pelvic pain, and frequent urination. Occasionally, these symptoms can become debilitating enough to have a negative impact on daily life.
In some instances, fibroids may also:
- Cause anemia
- Affect fertility
- Prevent pregnancy
- Result in pregnancy complications
Developing one fibroid also raises your risk of developing additional growths over time, although this risk drops off sharply during menopause.
If your doctor is evaluating you for fibroids, they are likely trying to determine the number, size, and location of any growths and their impact on nearby structures, including the bladder and kidneys. Understanding the full picture of your condition will help your doctor recommend the best treatment options, which might include medication, lifestyle changes, or, surgery.
History
If you have a longstanding relationship with your provider, they may already be familiar with your health and background. Either way, they will likely ask you questions like:
- How often do you get your periods?
- How long do your periods usually last?
- How heavy is the bleeding during your periods?
- Have you had any gynecological surgeries or procedures in the past?
- Do you experience pain or fever, particularly during your menstrual cycle?
- Do you notice a lot of clots during your periods?
- Is there a history of fibroids or other gynecological conditions in your family?
These questions help your doctor evaluate your risk and better understand your condition, but it’s okay if you don’t have all the answers! Many women don’t pay much attention to their periods and exact details like dates until they experience some kind of problem or change.
Physical Examination
If your doctor suspects a fibroid based on your symptoms or identifies risk factors in your medical history, they may want to do a pelvic and abdominal exam. This can feel a little bit awkward and uncomfortable at first but provides important information about your health that isn’t easy to obtain in other ways.
Abdominal Exam
During the first part of the exam, your doctor will get you to lie flat on the table and press down gently on different areas of your abdomen. This will typically include the upper abdomen, mid-stomach, pelvis, and groin.
Your provider is looking for any unusual masses or signs of enlargement. While rare, this might suggest the presence of larger fibroids that could be impacting nearby organs.
Pelvic Exam
The second part of this process is a pelvic examination. Sometimes, it’s easier for your doctor to feel fibroids from inside the vaginal canal, especially if they’re positioned near the cervix or near the neck of the uterus.
A pelvic exam follows the same process as a pap smear. Your doctor will start by having you change into a gown and lie down on the table, and a nurse may come in to help you feel more comfortable.
After informing you of the process and getting your consent, your doctor will insert two fingers into your vagina while pressing down on your abdomen with the other hand. This may be a bit uncomfortable, but shouldn’t be painful.
If fibroids are present, they will often feel like firm, irregular masses. You may notice tenderness over the spot when your doctor palpates the area, or you may not notice any symptoms at all.
Imaging
Imaging is an excellent way to confirm the presence of fibroids and can also help determine their size and location. Ultrasound, sonohysterogram, CT Scans, and MRIs can also be useful for assessing surrounding structures, like the kidneys and ureters, which can be affected by larger fibroids and increased pressure in the abdomen.
- Ultrasound is the most common type of imaging used in the diagnosis of fibroids. Your doctor may order a pelvic ultrasound, which is performed by moving a device over the outer abdomen, or a transvaginal ultrasound, which involves inserting a thin wand into the vagina to more easily identify any unusual masses.
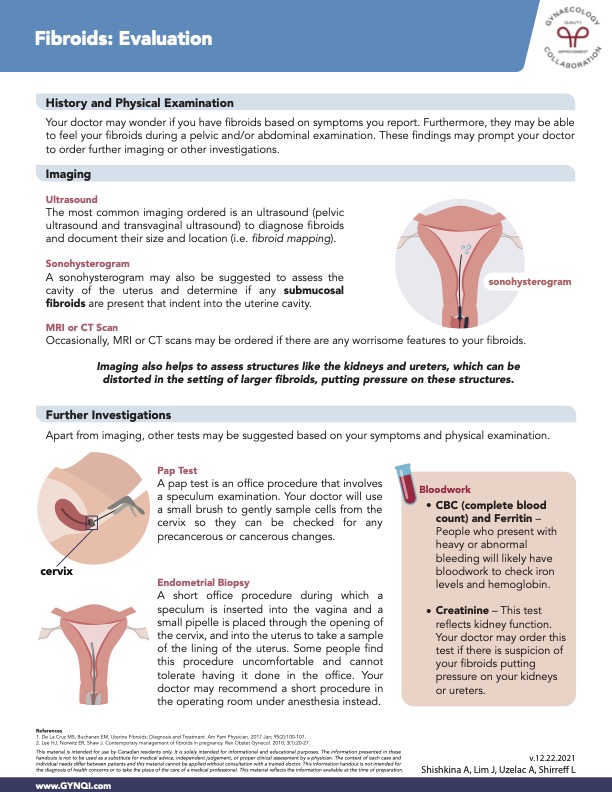
- Sonohysterogram may also be suggested to assess the cavity of the uterus and determine if any submucosal fibroids are present that indent into the uterine cavity. This is similar to a transvaginal ultrasound, but the technician will use a very small catheter to inject a few tablespoons of saline into your uterus first.
- Computerized Tomography (CT) Scan: While doctors do sometimes order CT scans for fibroid diagnosis, this is typically only useful for identifying calcified fibroids. You’ll lie down on the bed of the machine, which will move back and forth through an archway while taking images of your abdomen.
- MRI: Occasionally, MRI or CT scans may be ordered if there are any worrisome features to your fibroids. During this procedure, you’ll lie down on a table that slides into a long tube while the MRI machine uses magnetic fields to create detailed images of your uterus. The process can be a bit noisy, but isn’t uncomfortable.
No two imaging tests are exactly the same. Your doctor may recommend one type of imaging over another. Or, they may determine that you need multiple tests to confirm a diagnosis.
Further Investigations
Period Tracking
If you are not already tracking your periods, your doctor may suggest that you start. You can use a period-tracking app or just write down your start date, end date, and other important info about your flow and symptoms. This will help your doctor pinpoint any changes or patterns that might suggest you have fibroids.
Pap Test
If you haven’t had a pap test in a while, your doctor may recommend having this step taken care of during your initial physical exam.
A pap test is an office procedure that involves a speculum examination. Your doctor will use a small brush to gently sample cells from the cervix so they can be checked for any precancerous or cancerous changes.
Endometrial Biopsy
Endometrial biopsy is a short office procedure during which a speculum is inserted into the vagina. A small pipelle is placed through the opening of the cervix and into the uterus to take a sample of the lining of the uterus.
Some people find this procedure uncomfortable and cannot tolerate having it done in the office. Your doctor may recommend a short procedure in the operating room under twilight sedation or general anesthesia instead.
Bloodwork
People who present with heavy or abnormal bleeding will likely have bloodwork to check iron levels and hemoglobin. Your doctor may order a CBC (complete blood count) or other tests, like a Serum iron test, Transferrin test, or Total iron-binding capacity (TIBC) test.
Creatinine
This test reflects kidney function. Your doctor may order this test if there is suspicion of your fibroids putting pressure on your kidneys, bladder, or ureters, as this can raise your risk for urinary tract infections and kidney stones.
Should All Fibroids Be Treated?
Fibroids are generally only treated if they are causing problems or having a negative effect on your cycle, fertility, or health. Your doctor may recommend just keeping a close eye on your fibroids if they are very small or low in number.
It is more common for a person who develops a single fibroid to develop more over time. But some women will only ever develop 1-2, and in some cases, they eventually disappear. Monitoring how your fibroids develop over the first six to 12 months can help predict what outcome you’re more likely to face.
If your doctor does decide to treat your fibroids, they may suggest:
- Oral hormone medications
- Hormone-based IUD devices
- Revision (fibroid removal)
- Hysterectomy
Hysterectomy is typically reserved for severe cases that don’t respond to any other form of treatment and/or women who don’t intend to have any more children. Other treatments can provide equally effective relief from chronic pain, cramps, and excessive bleeding.



