Gestational Diabetes Screening
Diabetes mellitus (“diabetes”), is a disorder of glucose (sugar) regulation in the blood stream. Gestational diabetes mellitus (GDM) is a version of diabetes where you develop diabetes for the first time in pregnancy. This is because pregnancy hormones can cause the body to be resistant to insulin, the hormone that typically regulates blood sugar levels. This leads to elevated blood sugars that can negatively impact a pregnant person and baby. It typically arises in the second or third trimester. In Ontario, gestational diabetes can affect around 10% of pregnant people. We can screen for this condition using simple blood tests and a diagnosis and treatment can help reduce dangerous outcomes for the pregnant person and baby.
All pregnant people are offered screening for gestational diabetes between 24-28 weeks gestational age. If at high risk for GDM, screening may be offered earlier.
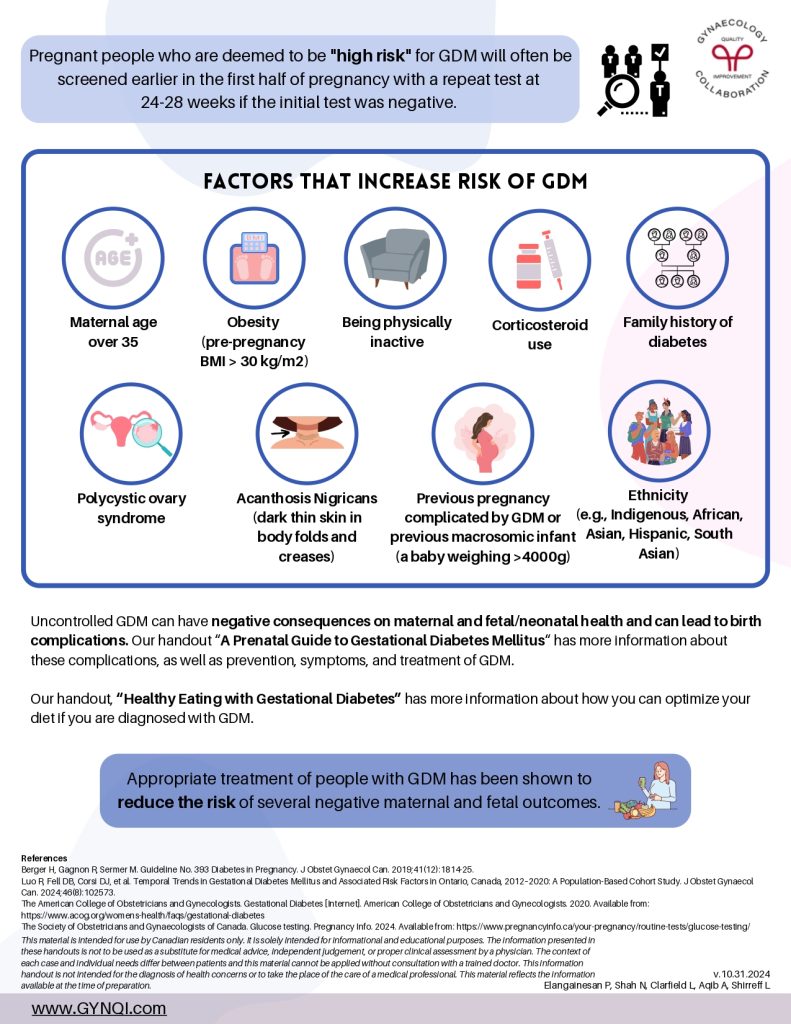
Screening Approach to GDM
Preferred 2-Step Screening and Diagnostic Approach
1 hour 50g glucose challenge test (GCT): Started at 24-28 weeks gestation at any time of day or earlier if high risk
- Normal GCS: <7.8 mmol/L → routine prenatal care (no gestational diabetes)
- Abnormal GCS: 7.8-11.0 mmol/L → 2h 75g oral glucose tolerance test (OGTT)
- Normal OGTT → routine prenatal care (no gestational diabetes)
- Any abnormal OGTT value: FPG ≥5,3; PG 1h ≥10.6; PG 2h ≥9.0 → gestational diabetes mellitus
- Abnormal GCS: ≥11.0 mmol/L → gestational diabetes mellitus
Alternative 1-Step Diagnostic Approach
2 hour 75g oral glucose tolerance test (OGTT): Started at 24-28 weeks gestation at any time of day or earlier if high risk
- Ant abnormal OGTT value: FPG ≥5.1; PG 1h ≥190; PG 2h ≥8.5 → gestational diabetes mellitus
- Normal OGTT → routine prenatal care (no gestational diabetes)
Note: FPG – fasting plasma glucose; PG – plasma glucose
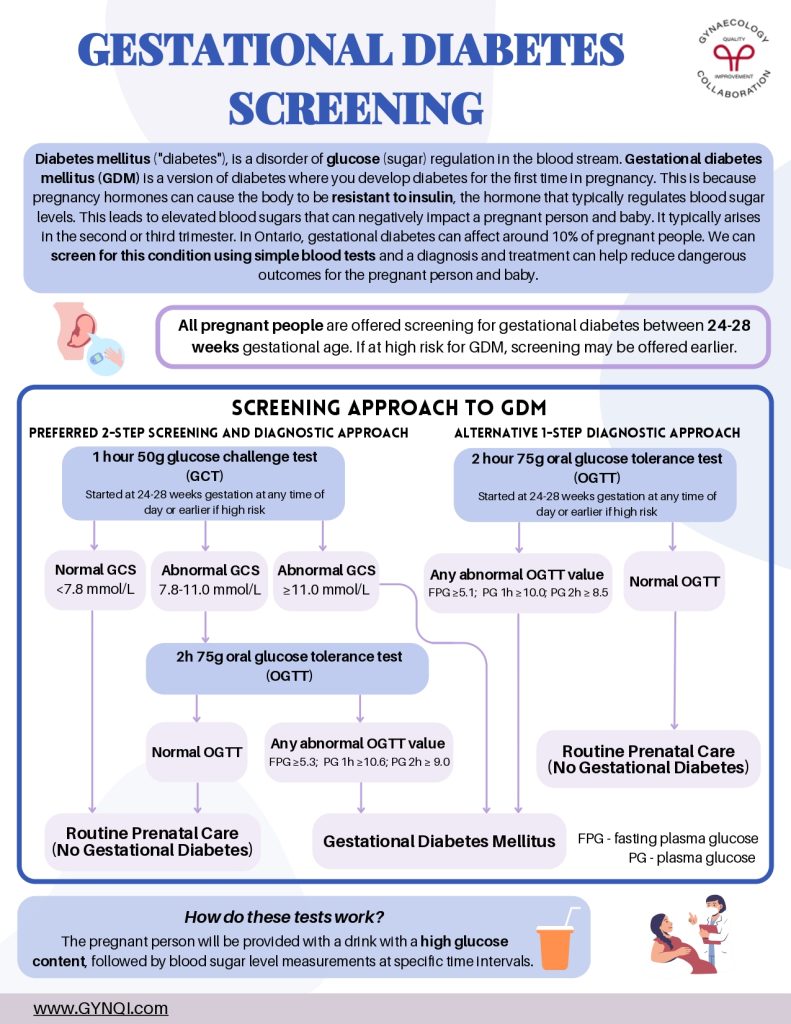
Pregnant people who are deemed to be “high risk” for GDM will often be screened earlier in the first half of pregnancy with a repeat test at 24-28 weeks if the initial test was negative.
Factors that Increase Risk of GDM
- Maternal age over 35
- Obesity (pre-pregnancy BMI >30kg/m2)
- Being physically inactive
- Corticosteroid use
- Family history of diabetes
- Polycystic ovary syndrome
- Acanthosis Nigricans (dark thin skin in body folds and creases)
- Previous pregnancy complicated by GDM or previous macrosomic infant (a baby weighing >4000g)
- Ethnicity (e.g., Indigenous, African, Asian, Hispanic, South Asian)
Uncontrolled GDM can have negative consequences on maternal and fetal/neonatal health and can lead to birth complications. Our handout “A Prenatal Guide to Gestational Diabetes Mellitus” has more information about these complications, as well as prevention, symptoms, and treatment of GDM.
Our handout, “Healthy Eating with Gestational Diabetes” has more information about how you can optimize your diet if you are diagnosed with GDM.
Appropriate treatment of people with GDM has been shown to reduce the risk of several negative maternal and fetal outcomes.