A Prenatal Guide To Gestational Diabetes Mellitus
01 What Is Gestational Diabetes?
Gestational diabetes mellitus (GDM) is a type of diabetes that may develop in 2-10% of pregnancies. During pregnancy, the body goes through hormonal changes that can make it harder for the body to use insulin effectively. Insulin is a hormone that helps regulate blood sugar levels. When a pregnant person’s body does not respond to insulin properly, it can lead to high levels of sugar in the blood, which is can lead to GDM. This condition usually develops in the second or third trimester of pregnancy and often goes away after the baby is born.
02 How Is Gestational Diabetes Diagnosed?
Screening (our handout “Gestational Diabetes Screening“ has more information): All pregnant individuals are offered screening between weeks 24-28 weeks of pregnancy. This may vary slightly depending on patient factors.
Follow-up Test (if needed): If the initial screening shows high blood sugar levels, your health care provider will recommend the Oral Glucose Tolerance Test (OGTT).
Diagnosis: Based on the results of the GCT or OGTT, your health care provider will determine if you have GDM. If you have it, your health care team will help you manage your blood sugar levels throughout the rest of your pregnancy to keep you and your baby healthy.
03 How Will Gestational Diabetes Affect Me and My Baby?
For you (the birthing parent):
- Gestational diabetes can increase the risk of certain pregnancy complications, such as high blood pressure (gestational hypertension or pre-eclampsia), need for a Caesarean section (C-section) delivery, more severe tearing during delivery, miscarriage, difficulties with sugar control (too high or too low can cause symptoms and illness), infection (urinary tract infection, upper respiratory tract infection, wound infection), and a more severe, but rare, complication of diabetes called diabetic ketoacidosis.
- Having gestational diabetes can increase your chances of developing type 2 diabetes later in life. It’s therefore essential to maintain a healthy lifestyle and to follow up with recommended screening.
For your baby:
- Neonatal/fetal risks: congenital anomalies, increased growth of the baby (macrosomia), increased amniotic fluid around the baby (polyhydramnios), preterm labour, fetal/neonatal trauma during the delivery, the baby getting stuck during delivery (dystocia), delayed fetal lung maturity, and stillbirth
- After birth, the baby may have low blood sugar levels (hypoglycemia) because their body is still producing insulin to handle the higher blood sugar levels from the birthing parent.
- Babies have a higher risk of developing:
- Respiratory distress syndrome (RDS), a condition that affects breathing.
- Type 2 diabetes later in life.
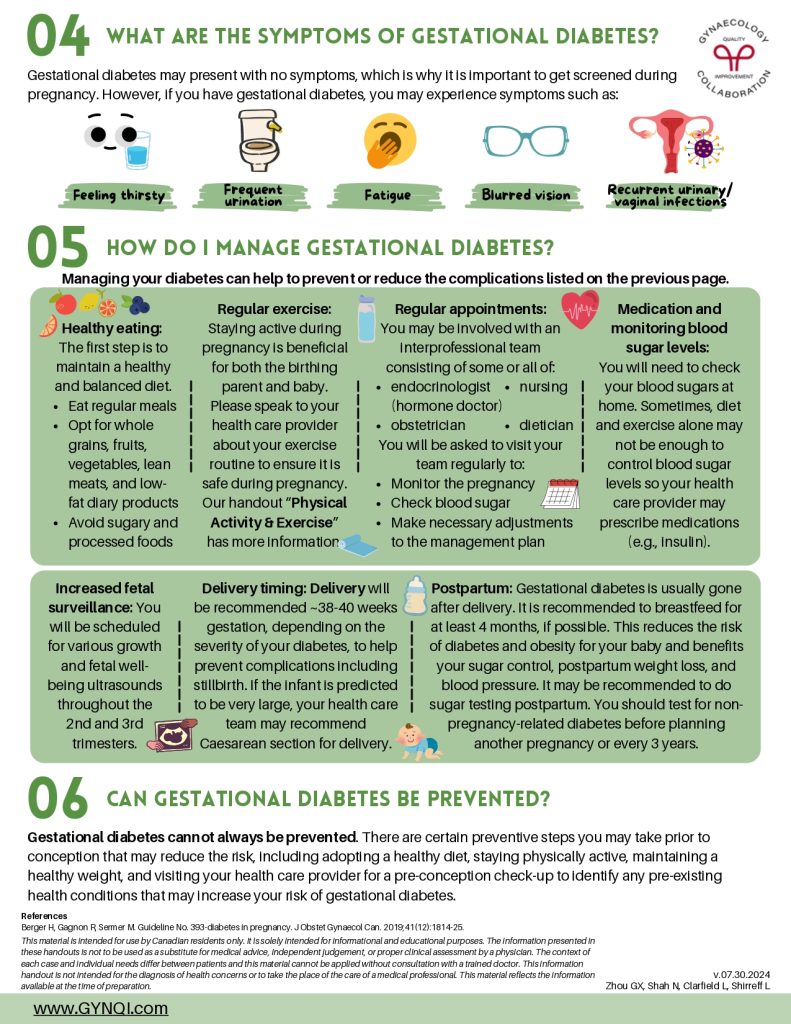
04 What Are the Symptoms of Gestational Diabetes?
Gestational diabetes may present with no symptoms, which is why it is important to get screened during pregnancy. However, if you have gestational diabetes, you may experience symptoms such as:
- Feeling thirsty
- Frequent urination
- Fatigue
- Blurred vision
- Recurrent urinary/vaginal infections
05 How Do I Manage Gestational Diabetes?
Managing your diabetes can help to prevent or reduce the complications listed on the previous page.
Healthy eating: The first step is to maintain a healthy and balanced diet.
- Eat regular meals
- Opt for whole grains, fruits, vegetables, lean meats, and low-fat dairy products
- Avoid sugary and process foods
Regular exercise: Staying active during pregnancy is beneficial for both the birthing parent and baby. Please speak to your health care provider about your exercise routine to ensure it is safe during pregnancy. Our handout “Physical Activity & Exercise” has more information.
Regular appointments: You may be involved with an interprofessional team consisting of some or all of:
- Endocrinologist (hormone doctor)
- Obstetrician
- Nursing
- Dietician
You will be asked to visit your team regularly to:
- Monitor the pregnancy
- Check blood sugar
- Make necessary adjustments to the management plan
Medication and monitor blood sugar levels: You will need to check your blood sugars at home. Sometimes, diet and exercise alone may not be enough to control blood sugar levels so your health care provider may prescribe medications (e.g., insulin).
Increased fetal surveillance: You will be scheduled for various growth and fetal well-being ultrasounds throughout the 2nd and 3rd trimesters.
Delivery timing: Delivery will be recommended ~38-40 weeks gestation, depending on the severity of your diabetes, to help prevent complications including stillbirth. If the infant is predicted to be very large, your health care team may recommend Caesarean section for delivery.
Postpartum: Gestational diabetes is usually gone after delivery. It is recommended to breastfeed for at least 4 months, if possible. This reduces the risk of diabetes and obesity for your baby and benefits your sugar control, postpartum weight loss, and blood pressure. It may be recommended to do sugar testing postpartum. You should test for non-pregnancy-related diabetes before planning another pregnancy or every 3 years.
06 Can Gestational Diabetes Be Prevented?
Gestational diabetes cannot always be prevented. There are certain preventive steps you may take prior to conception that may reduce the risk, including adopting a healthy diet, staying physically active, maintaining a healthy weight, and visiting your health care provider for a pre-conception check-up to identify any pre-existing health conditions that may increase your risk of gestational diabetes.