You Have Iron Deficiency (and You're Pregnant)
1. What is Iron Deficiency?
Iron is an essential mineral that your body needs for growth and development. It is an important component of hemoglobin, a protein in red blood cells that transports oxygen around the body. When your body does not have enough iron, your hemoglobin levels can drop below normal, and your organs are unable to get the adequate amount of oxygen they require. This condition is known as iron deficiency anemia. It is the most common form of anemia. A lack of iron can lead to many symptoms and impair your ability to do normal daily activities.
2. Why is iron important during pregnancy?
Iron deficiency occurs in over 30% of pregnancies in Canada.
Symptoms of iron deficiency are often dismissed as normal
pregnancy symptoms. Many patients are left untreated, which increases the health risks for both mom (heavy bleeding at delivery, need for blood transfusion) and baby (smaller size, preterm birth). There is even some information that it may have long-term effects on the baby’s brain development
3. Will eating more iron-rich foods help?
A dietary strategy works best for prevention rather than treatment of iron deficiency.
| Heme iron-containing foods | Lean red meat, chicken, fish, pork, shrimp |
| Non-heme ironcontaining foods | Beans, leafy greens, dried fruits, eggs, wholemeal bread, iron-fortified breakfast cereals |
4. What are my treatment options?
Iron deficiency can be treated.
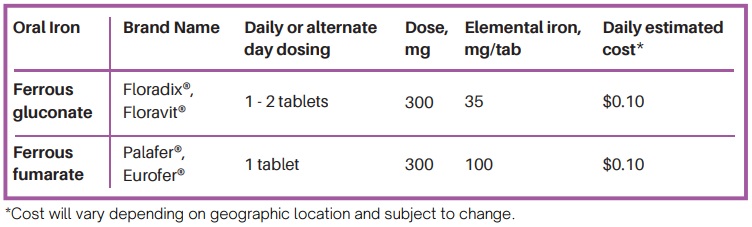
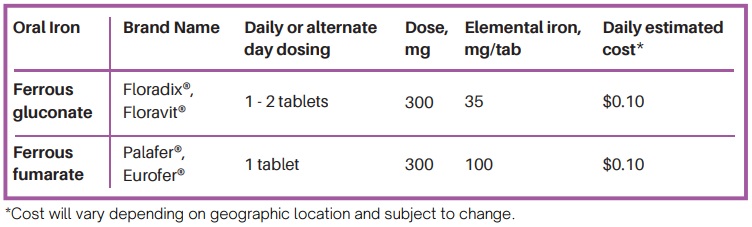
Oral iron supplements, taken by mouth and absorbed through the digestive tract, are the first choice in treatment for most patients. Iron supplements are “over the counter” and do not require a prescription. There are many iron preparations available including pills, capsules, drops, and extended-release tablets (Table 1). If you have iron deficiency in pregnancy, prenatal vitamins do not have enough iron to correct the deficiency and an additional iron supplement will be required. Typically, adults will need to take between 60-120mg of elemental iron per day.
Intravenous (IV) iron infusion is an alternative treatment option to oral iron that can supplement iron at a much faster rate. It is safe and effective in the second and third trimester and during breastfeeding. It may be recommended by your doctor as an alternative option in cases where oral iron is not tolerated, not able to correct iron deficiency, or where iron is needed quickly (like close to the time of birth).
Table 1: Some commonly recommended oral iron products
5. How should I take my oral iron?
MAXIMIZE IRON ABSORPTION
Take your iron supplements on an empty stomach (preferably 1-2
hours before a meal) with vitamin C.
Vitamin C can be in the form of a supplement (250-500mg) or a citrus drink (e.g. orange juice).
AVOID CERTAIN FOODS AND MEDICATIONS
Avoid these within 1 hour of oral iron:
- Calcium
- Proton pump inhibitors (e.g.
omeprazole, pantoprozole) - Antacids (e.g. Tums, Gaviscon,
famotidine) - Thyroid medication
- Tea, coffee, milk
- Soy
- Eggs
WATER AND FIBRE
Consume lots of water and fibre with your iron to reduce constipation and cramping side effects. If you have constipation, try taking a laxative such as Senokot or PEG.
If the side effects of oral iron are very bothersome, you can try taking your iron supplement EVERY OTHER DAY.
6. What are the side effects of oral iron?
- Dark stools
- Stomach discomfort
- Nausea
- Diarrhea
- Constipation
These side effects are bothersome but not dangerous.
Side effects can be lessened by:
- Drinking lots of water
- Increasing fibre in diet (e.g. Metamucil, bran, vegetables)
- Taking iron before bedtime
- Taking a stool softener
- Changing to ‘every other day’ dosing
7. What happens now?
It is recommended that you repeat your blood tests 2-4 weeks after the start of your iron supplement to ensure that you are responding to treatment. Once your hemoglobin and iron levels are normalized, you may need to take the iron supplement for another six months.
For more information, talk to your doctor. Always consult with your doctor about the treatment plan that is right for you.
You Have Iron Deficiency (and You're Having Surgery)
1. What is Iron Deficiency?
Iron is an essential mineral that your body needs for growth and development. It is an important component of hemoglobin, a protein in red blood cells that transports oxygen around the body. When your body does not have enough iron, your hemoglobin levels can drop below normal, and your organs are unable to get the adequate amount of oxygen they require. This condition is known as iron deficiency anemia. It is the most common form of anemia. A lack of iron can lead to many symptoms and impair your ability to do normal daily activities.
2. Why is it important to correct iron levels prior to surgery?
It is ideal for people to go into surgery with a hemoglobin level greater than 120 g/L.
People with iron deficiency anemia are more likely to require blood transfusions around the time of their surgery, get an infection, have a longer hospital stay, and be at an increased risk of complications, readmission to hospital, and rarely, death. It is very important to correct
iron deficiency before individuals undergo surgery to ensure the best health outcomes.
3. Will eating more iron-rich foods help?
A dietary strategy works best for prevention rather than treatment of iron deficiency.
While eating an iron-rich diet can help to prevent iron deficiency anemia, an average person’s intake of dietary iron is not enough to correct the condition once it has developed. There are two main sources of iron in our diets: animal (heme iron) and plant (non-heme).
| Heme iron-containing foods | Lean red meat, chicken, fish, pork, shrimp |
| Non-heme ironcontaining foods | Beans, leafy greens, dried fruits, eggs, wholemeal bread, iron-fortified breakfast cereals |
4. What are my treatment options?
Iron deficiency can be treated.
Oral iron supplements, taken by mouth and absorbed through the digestive tract, are the first choice in treatment for most patients. Iron supplements are “over the counter” and do not require a prescription. There are many iron preparations available including pills, capsules, drops, and extended-release tablets (Table 1). If you have iron deficiency in pregnancy, prenatal vitamins do not have enough iron to correct the deficiency and an additional iron supplement will be required. Typically, adults will need to take between 60-120mg of elemental iron per day.
Intravenous (IV) iron infusion is an alternative treatment option to oral iron that can supplement iron at a much faster rate. It may be recommended by your doctor as an alternative option in cases where oral iron is not tolerated, not able to correct iron deficiency, or where iron is needed quickly (like close to the time of birth).
Table 1: Some commonly recommended oral iron products
5. How should I take my oral iron?
MAXIMIZE IRON ABSORPTION
Take your iron supplements on an empty stomach (preferably 1-2
hours before a meal) with vitamin C.
Vitamin C can be in the form of a supplement (250-500mg) or a citrus drink (e.g. orange juice).
AVOID CERTAIN FOODS AND MEDICATIONS
Avoid these within 1 hour of oral iron:
- Calcium
- Proton pump inhibitors (e.g.
omeprazole, pantoprozole) - Antacids (e.g. Tums, Gaviscon,
famotidine) - Thyroid medication
- Tea, coffee, milk
- Soy
- Eggs
WATER AND FIBRE
Consume lots of water and fibre with your iron to reduce constipation and cramping side effects. If you have constipation, try taking a laxative such as Senokot or PEG.
If the side effects of oral iron are very bothersome, you can try taking your iron supplement EVERY OTHER DAY.
6. What are the side effects of oral iron?
- Dark stools
- Stomach discomfort
- Nausea
- Diarrhea
- Constipation
These side effects are bothersome but not dangerous.
Side effects can be lessened by:
- Drinking lots of water
- Increasing fibre in diet (e.g. Metamucil, bran, vegetables)
- Taking iron before bedtime
- Taking a stool softener
- Changing to ‘every other day’ dosing
7. What happens now?
It is recommended that you repeat your blood tests 2-4 weeks after the start of your iron supplement to ensure that you are responding to treatment. Once your hemoglobin and iron levels are normalized, you may need to take the iron supplement for another six months.
For more information, talk to your doctor. Always consult with your doctor about the treatment plan that is right for you.