
Table of Contents
- Summary
- What is Polycystic Ovary Syndrome (PCOS)?
- Symptoms of PCOS
- Menstrual Irregularities
- Hyperandrogenism
- Fertility Concerns
- Weight Gain and Obesity
- Diagnosis of PCOS
- What Can Happen in Polycystic Ovary Syndrome?
- Excess Androgens
- Insulin Resistance
- Thickening of Endometrial Lining
- Anovulation
- Treatment of PCOS
- Long-Term Health Risks of PCOS
- An Overview of Managing PCOS
Summary:
- Polycystic Ovary Syndrome (PCOS) is a common hormonal disorder affecting 5-8% of women in Canada, characterized by irregular menstrual cycles, elevated androgen levels, and difficulties with weight management.
- Individuals with PCOS may experience a range of symptoms, including acne, excessive facial or body hair, thinning hair on the scalp, irregular periods, and fertility challenges.
- A diagnosis of PCOS typically requires at least two of the following three criteria: menstrual irregularities, elevated androgen levels, and imaging results showing ovaries with multiple small cysts.
- While PCOS cannot be cured, treatment options such as lifestyle changes, hormonal contraception, and medications can help manage symptoms and reduce long-term health risks.
Polycystic Ovary Syndrome (PCOS) is a complex hormonal disorder that affects a significant number of women, with approximately 5-8% impacted in Canada alone. Characterized by irregular menstrual cycles, elevated androgen levels, and challenges with weight management, PCOS can lead to a range of symptoms, including acne and excess facial or body hair.
Symptoms can vary widely among those affected, making PCOS a highly individualized condition.
What is Polycystic Ovary Syndrome (PCOS)?
Polycystic ovary syndrome (PCOS) is a condition characterized by irregular menstrual cycles, challenges with weight loss, and elevated levels of androgenic hormones, such as testosterone. This can result in symptoms like acne, excess facial or body hair, and thinning hair on the scalp.
Additionally, PCOS can complicate the process of conception. It is a prevalent condition, affecting approximately 5-8% of women in Canada.
Symptoms of PCOS
Symptoms of PCOS can vary significantly from person to person, making it a highly individualized condition.
Menstrual Irregularities
Experiencing fewer than eight menstrual periods per year (a condition known as oligomenorrhea or amenorrhea).
Hyperandrogenism
Elevated levels of male hormones, such as testosterone, can manifest in several ways, including:
- Acne
- Development of thick, dark hair on areas such as the upper lip, chin, sideburns, chest, and abdomen
- Hair loss on the scalp
Fertility Concerns
Difficulty conceiving may occur without the use of ovulation induction medications, such as Clomid or Letrozole, to assist with the ovulation process.
Weight Gain and Obesity
Those with PCOS often experience issues with hormonal imbalances, metabolism, and as a result, weight gain.
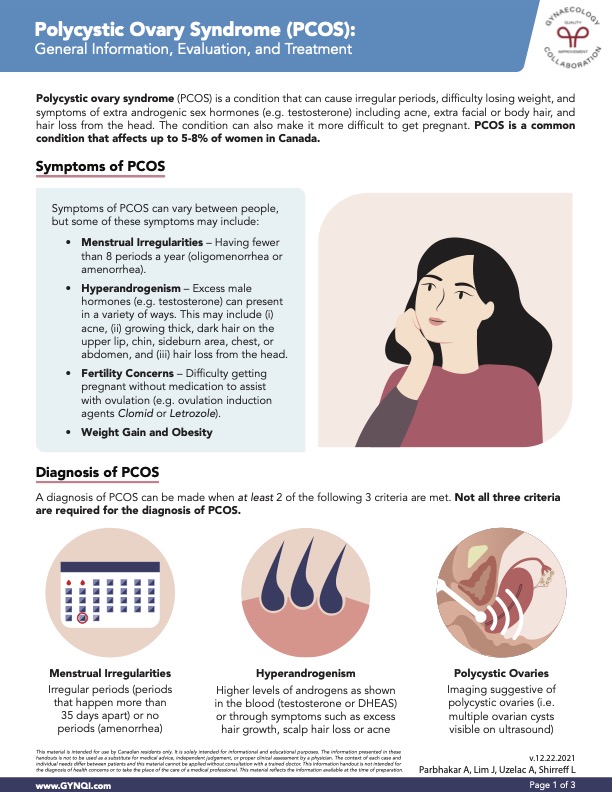
Diagnosis of PCOS
A diagnosis of PCOS is made when at least two of the following three criteria are met, though it is not necessary for all three criteria to be fulfilled.
- Menstrual Irregularities: Irregular periods (periods that happen more than 35 days apart) or no periods (amenorrhea).
- Hyperandrogenism: Elevated levels of androgens, such as testosterone or DHEAS, are indicated by blood tests or manifested through symptoms like excessive hair growth, hair loss on the scalp, or acne.
- Polycystic Ovaries: Imaging findings indicative of polycystic ovaries, characterized by the presence of multiple ovarian cysts visible on ultrasound.
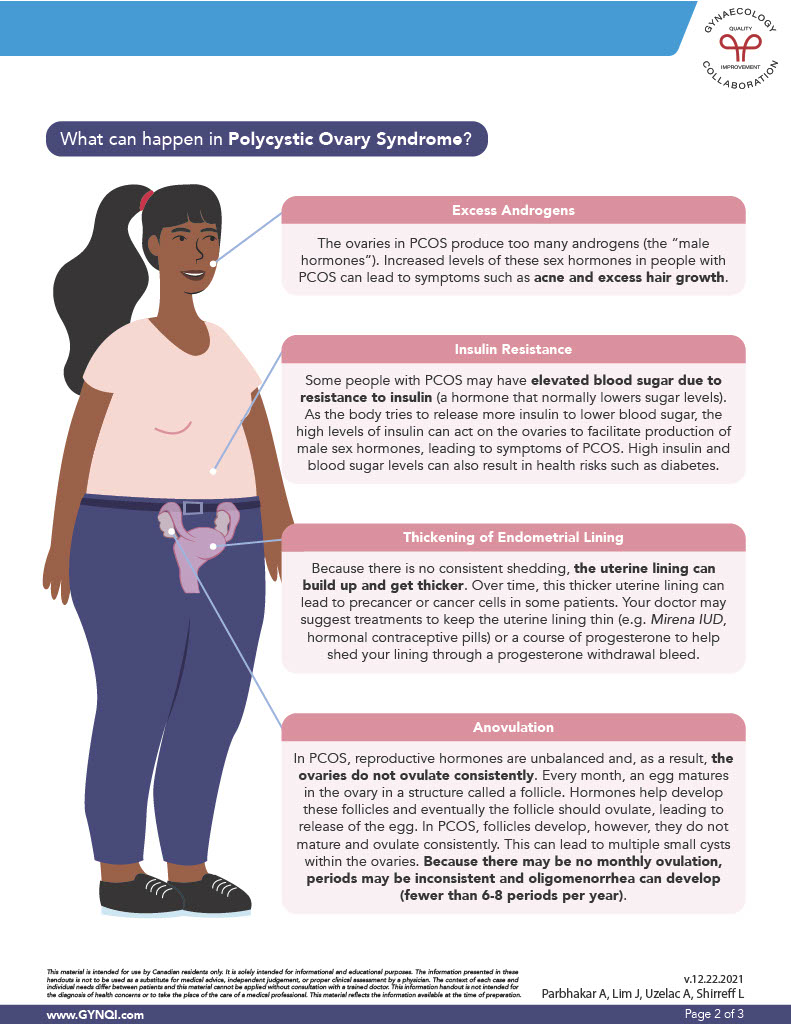
What Can Happen in Polycystic Ovary Syndrome?
Excess Androgens
In PCOS, the ovaries produce an excess of androgens, or “male hormones.” Elevated levels of these hormones can result in symptoms such as acne and excessive hair growth.
Insulin Resistance
Individuals with PCOS may experience elevated blood sugar due to insulin resistance, the hormone that normally lowers sugar levels. This resistance prompts the body to produce more insulin, which can stimulate the ovaries to produce excess male hormones, exacerbating PCOS symptoms. Elevated insulin and blood sugar levels also increase the risk of developing diabetes.
Thickening of Endometrial Lining
Due to the lack of regular shedding, the uterine lining can build up and become thicker over time. This thickened lining may increase the risk of developing precancerous or cancerous cells in some patients.
To manage this, your doctor may recommend treatments to help maintain a thinner uterine lining, such as the Mirena IUD or hormonal contraceptive pills, or a course of progesterone to induce shedding through a progesterone withdrawal bleed.
Anovulation
PCOS causes hormonal imbalances that prevent the ovaries from ovulating regularly. Typically, each month an egg matures within a structure called a follicle in the ovary. Hormones are responsible for developing these follicles and triggering ovulation, which releases the egg. In PCOS, this process is often disrupted, leading to inconsistent ovulation.
In PCOS, follicles begin to develop but often fail to mature and ovulate consistently. This can result in multiple small cysts forming in the ovaries. Without regular ovulation, menstrual cycles can become irregular, leading to oligomenorrhea (fewer than 6-8 periods per year).
Treatment of PCOS
PCOS cannot be cured, but a range of treatments is available to manage its symptoms and related issues. Treatment plans should be tailored to each individual’s symptoms, overall health, and future pregnancy goals.
Lifestyle Changes: Weight loss through diet and exercise in people with PCOS who are overweight improves insulin resistance, lowers cholesterol, and reduces symptoms like excess hair growth. It can also positively impact ovulation and fertility.
Combined Hormonal Contraception: Combined hormonal contraception, such as birth control pills, does not cure PCOS but can help manage symptoms like irregular periods, acne, and facial hair. It also promotes regular shedding of the uterine lining, reducing the risk of precancerous or cancerous changes in the uterus.
Progesterone IUDs: Progesterone IUDs, like Mirena or Kyleena, help maintain a thin uterine lining, reducing the risk of developing precancerous or cancerous cells in the uterus.
Spironolactone: Spironolactone is commonly prescribed to manage symptoms of excess androgens, such as acne, facial hair, and excessive body hair.
Metformin: Metformin is used to help the body respond to insulin. In people with PCOS, it can help improve ovulation and decrease androgen levels.
Acne Treatment: Medicated creams or antibiotics can be used alongside other treatments to help manage acne.
Hair Removal: Permanent hair removal methods, such as laser therapy or electrolysis, can be effective in managing excess hair growth.
Long-Term Health Risks of PCOS
Addressing PCOS through lifestyle changes and appropriate medical interventions can help mitigate risks and improve your overall health.
Long-term health risks can include:
- Insulin resistance can increase the risk of developing type 2 diabetes and cardiovascular disease
- Higher cholesterol levels and metabolic syndrome
- Sleep apnea (a sleep disorder characterized by brief interruptions in breathing during sleep)
- Endometrial hyperplasia, which can increase the risk of endometrial cancer
- Depression
An Overview of Managing PCOS
Polycystic Ovary Syndrome (PCOS) is a prevalent condition characterized by irregular menstrual cycles, elevated androgen levels, and symptoms like acne and excess hair growth. Diagnosis is based on menstrual irregularities, hyperandrogenism, and imaging findings of polycystic ovaries.
While PCOS cannot be cured, various treatments can effectively manage symptoms and reduce long-term health risks. By adopting lifestyle changes and exploring medical options, individuals with PCOS can improve their well-being and navigate the complexities of this disorder.



