Prenatal Screening
This handout provides an overview of the techniques used to screen your baby for certain chromosomal abnormalities(a group of genetic conditions) during pregnancy. This handout is specific to pregnant people living in Ontario. Please refer to your provincial/territorial guidelines for local screening recommendations.
Screening tests are not “diagnostic” – they cannot confirm with certainty whether a condition is present or not. Instead, they indicate your baby’s risk level to help you decide whether to do further testing.
The timelines and information provided in this handout apply to singleton pregnancies. For pregnancies where there is more than one baby (e.g., twins or triplets), please consult your care team to see how guidance differs.
Enhanced First Trimester Screening (eFTS)
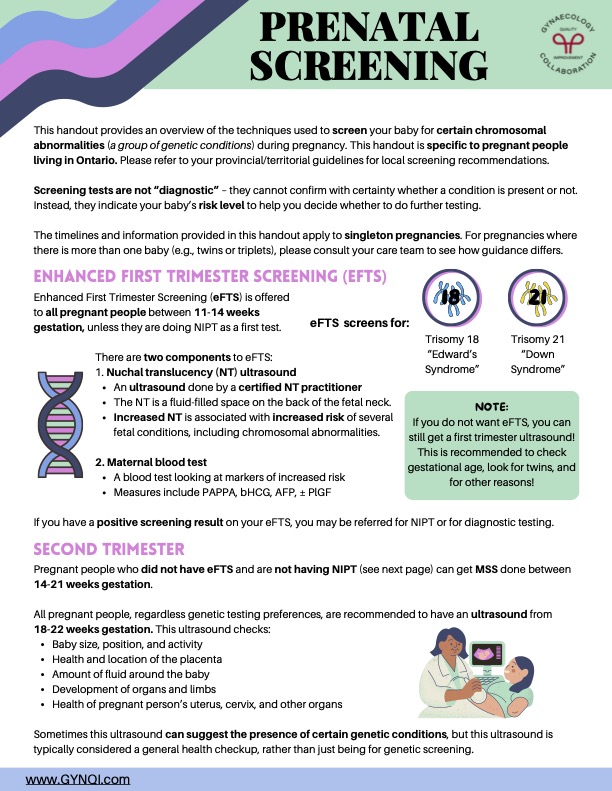
Enhanced First Trimester Screening (eFTS) is offered to all pregnant people between 11-14 weeks gestation, unless they are doing NIPT as a first test.
There are two components to eFTS:
There are two components to eFTS:
- Nuchal translucency (NT) ultrasound
- An ultrasound done by a certified NT practitioner
- The NT is a fluid-filled space on the back of the fetal neck.
- Increased NT is associated with increased risk of several fetal conditions, including chromosomal abnormalities.
- Maternal blood test
-
- A blood test looking at markers of increased risk
- Measures include PAPPA, bHCG, AFP, ± PlGF
eFTS screens for: Trisomy 18 “Edward’s Syndrome”, Trisomy 21 “Down Syndrome”
Note: If you do not want eFTS, you can still get a first trimester ultrasound! This is recommended to check gestational age, look for twins, and for other reasons!
If you have a positive screening result on your eFTS, you may be referred for NIPT or for diagnostic testing.
Second Trimester
Pregnant people who did not have eFTS and are not having NIPT (see next page) can get MSS done between 14-21 weeks gestation.
All pregnant people, regardless genetic testing preferences, are recommended to have an ultrasound from 18-22 weeks gestation. This ultrasound checks:
- Baby size, position, and activity
- Health and location of the placenta
- Amount of fluid around the baby
- Development of organs and limbs
- Health of pregnant person’s uterus, cervix, and other organs
Sometimes this ultrasound can suggest the presence of certain genetic conditions, but this ultrasound is typically considered a general health checkup, rather than just being for genetic screening.
Non-Invasive Prenatal Testing (NIPT)
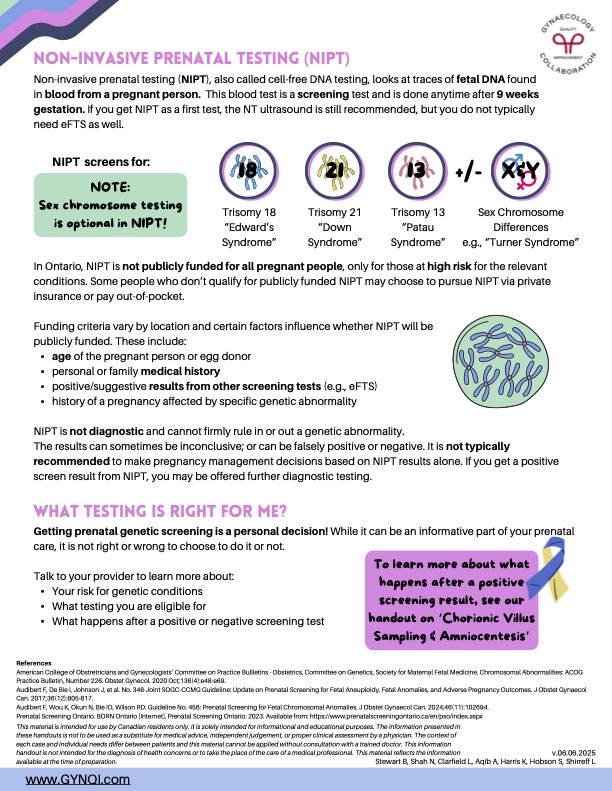
Non-invasive prenatal testing (NIPT), also called cell-free DNA testing, looks at traces of fetal DNA found in blood from a pregnant person. This blood test is a screening test and is done anytime after 9 weeks gestation. If you get NIPT as a first test, the NT ultrasound is still recommended, but you do not typically need eFTS as well.
NIPT screens for: Trisomy 18 “Edward’s Syndrome”, Trisomy 21 “Down Syndrome”, Trisomy 13 “Patau Syndrome”, +/- Sex Chromosome Differences (e.g., “Turner Syndrome”)
Note: sex chromosome testing is optional in NIPT!
In Ontario, NIPT is not publicly funded for all pregnant people, only for those at high risk for the relevant conditions. Some people who don’t qualify for publicly funded NIPT may choose to pursue NIPT via private insurance or pay out-of-pocket.
Funding criteria vary by location and certain factors influence whether NIPT will be publicly funded. These include:
- age of the pregnant person or egg donor
- personal or family medical history
- positive/suggestive results from other screening tests (e.g., eFTS)
- history of a pregnancy affected by specific genetic abnormality
NIPT is not diagnostic and cannot firmly rule in or out a genetic abnormality.
The results can sometimes be inconclusive; or can be falsely positive or negative. It is not typically recommended to make pregnancy management decisions based on NIPT results alone. If you get a positive screen result from NIPT, you may be offered further diagnostic testing.
What Testing is Right for Me?
Getting prenatal genetic screening is a personal decision! While it can be an informative part of your prenatal care, it is not right or wrong to choose to do it or not.
Talk to your provider to learn more about:
- Your risk for genetic conditions
- What testing you are eligible for
- What happens after a positive or negative screening test
To learn more about what happens after a positive screening result, see our handout on ‘Chorionic Villus Sampling & Amniocentesis’