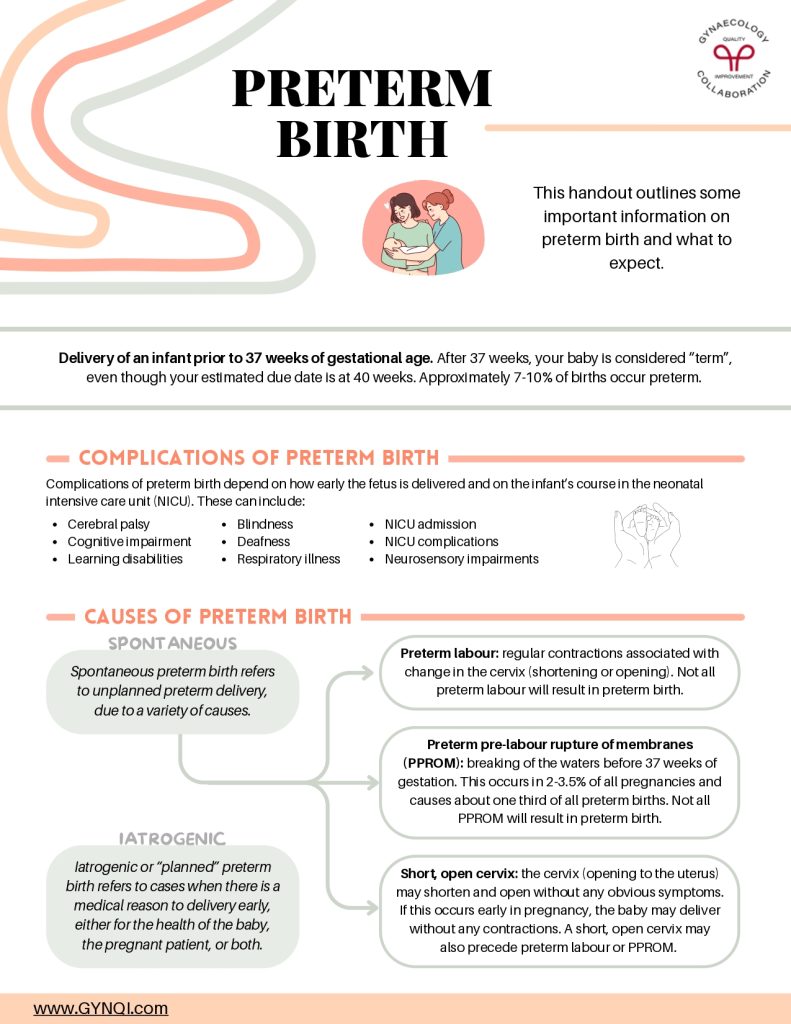
Preterm Birth
The handout outlines some important on preterm birth and what to expect.
Delivery of an infant prior to 37 weeks of gestational age. After 37 weeks, your baby is considered “term”, even though your estimated due date is at 40 weeks. Approximately 7-10% of births occur preterm.
Complications of Preterm Birth
Complications of preterm birth depend on how early the fetus is delivered and on the infant’s course in the neonatal intensive care unit (NICU). These can include:
- Cerebral palsy
- Cognitive impairment
- Learning disability
- Blindness
- Deafness
- Respiratory illness
- NICU admission
- NICU complications
- Neurosensory impairments
Causes of Preterm Birth
Spontaneous
Spontaneous preterm birth refers to unplanned preterm delivery, due to a variety of causes.
- Preterm labour: regular contractions associated with change in the cervix (shortening or opening). Not all preterm labour will result in preterm birth.
- Preterm pre-labour rupture of membranes (PPROM): breaking of the waters before 37 weeks of gestation. This occurs in 2-3.5% of all pregnancies and causes about one third of all preterm births. Not all PPROM will result in preterm birth.
- Short, open cervix: the cervix (opening to the uterus) may shorten and open without any obvious symptoms. If this occurs early in pregnancy, the baby may deliver without any contractions. A short, open cervix may also precede preterm labour or PPROM.
Iatrogenic
Iatrogenic or “planned” preterm birth refers to cases when there is a medical reason to delivery early, either for the health of the baby, the pregnant patient, or both.
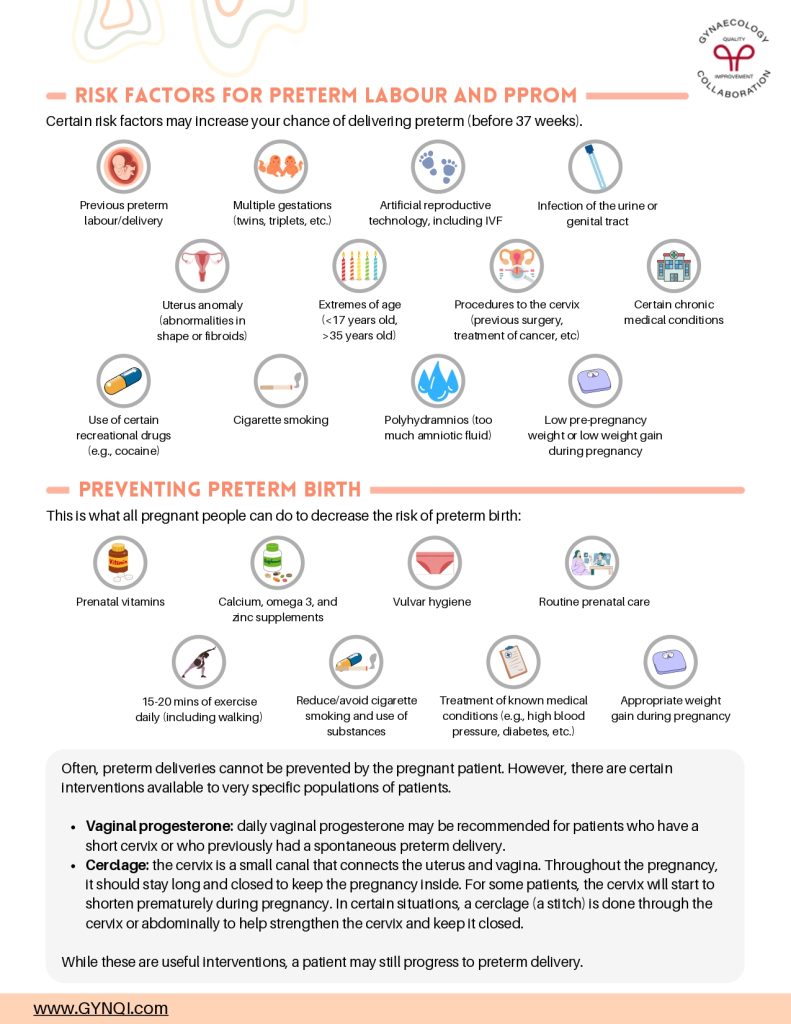
Risk Factors For Preterm Labour and PPROM
Certain risk factors may increase your chance of delivering preterm (before 37 weeks).
- Previous preterm labour/delivery
- Multiple gestations (twins, triplets, etc.)
- Artificial reproductive technology, including IVF
- Infection of the urine or genital tract
- Uterus anomaly (abnormalities in shape or fibroids)
- Extremes of age (<17 years old, >35 years old)
- Procedures to the cervix (previous surgery, treatment of cancer, etc.)
- Certain chronic medical conditions
- Use of certain recreational drugs (e.g., cocaine)
- Cigarette smoking
- Polyhydramnios (too much amniotic fluid)
- Low pre-pregnancy weight or low weight gain during pregnancy
Preventing Preterm Birth
This is what all pregnant people can do to decrease the risk of preterm birth:
- Prenatal vitamins
- Calcium, omega 3, and zinc supplements
- Vulvar hygiene
- Routine prenatal care
- 15-20 mins of exercise daily (including walking)
- Reduce/avoid cigarette smoking and use of substances
- Treatment of known medical conditions (e.g., high blood pressure, diabetes, etc.)
- Appropriate weight gain during pregnancy
Often, preterm deliveries cannot be prevented by the pregnant patient. However, there are certain interventions available to very specific populations of patients.
- Vaginal progesterone: daily vaginal progesterone may be recommended for patients who have a short cervix or who previously had a spontaneous preterm delivery.
- Cerclage: the cervix is a small canal that connects the uterus and vagina. Throughout the pregnancy, it should stay long and closed to keep the pregnancy inside. For some patients, the cervix will start to shorten prematurely during pregnancy. In certain situations, a cerclage (a stitch) is done through the cervix or abdominally to help strengthen the cervix and keep it closed.
While these are useful interventions, a patient may still progress to preterm delivery.
Management of Preterm Labour and PPROM
Antenatal corticosteroids: Injectable medication given over 2 days to patients who are at risk of delivering before 34 weeks. This helps with fetal lung maturity and has been proven to reduce the risk of perinatal death, respiratory distress syndrome, intraventricular hemorrhage (brain bleeding), and necrotizing enterocolitis (bowel issue).
Tocolysis: These medications are intended to slow down the progression of preterm labour so that there is enough time to administer the full dose of corticosteroids and/or transfer you to a hospital with appropriate NICU beds.
Magnesium sulphate: Intravenous medication if preterm delivery before 34 weeks is imminent over the next few hours. This is intended to help with protecting baby’s brain.
Antibiotics: These medications vary and may be given if your group B streptococcus status is unknown (typically tested around 35-36 weeks) and/or if your waters are broken. These antibiotics are intended to help prevent infections in baby and to treat any infections in the pregnant patient that may be the cause of preterm birth.
Observation on Labour & Delivery: Ideally, we delay or stop preterm labour from progressing. Sometimes, if labour is underway, we cannot slow it down or stop it. In this case, we may give the medications listed above to help prevent complications and to optimize baby for preterm delivery.
Admission to antepartum/antenatal unit: Sometimes, if you are stable and preterm labour settles, we may continue to monitor you on our antepartum or antenatal unit. This may range from several days to several weeks.
NICU: There are different levels of NICU, meaning they have varying abilities and infrastructure to take care of preterm babies. If your current hospital does not have the ability to care for very preterm babies, you and/or baby may be transferred to another hospital to ensure there is appropriate care, if this can be done safely.
Care team: Your care team may expand to OBGYN, maternal-fetal medicine specialists, and pediatrics (who will discuss what to expect if baby is born early). Social work and psychological support are also available as needed to help support you and your team.
Symptoms To Watch and Go To OB Triage For
- Consistent (regular) or painful uterine contractions or cramping. You will experience pain, and your uterus will feel hard. Painless, irregular cramping may be a normal part of pregnancy.
- Constant, dull low backache
- New pelvic pressure or fullness
- Gush of fluid from the vagina (clear, pink, bloody, or yellow-green) or ongoing slow trickle of fluids
- Sudden gush of honey-coloured vaginal discharge
- Spotting or bleeding from the vagina
- Sudden increase or fullness in vagina