Table of Contents
- Summary
- Systemic Menopausal Hormonal Therapy Basics
- What are the Different Ways to Take Estrogen and Progesterone
- Why Might I Need Progesterone?
- Combination Therapies
- Determining Dose of Systemic Menopause Hormonal Therapy
- How Long Does it Take for Systemic MHT to Work?
- When is the Best Time to Start and Stop Systemic MHT?
- How Do I Stop Taking My Systemic MHT?
- The Main Risks of Systemic MHT
- Blood Clots
- Breast Cancer
- Heart-Attack & Stroke
- An Effective Treatment for Managing Menopause Symptoms
Summary:
- Estrogen can be taken orally or applied transdermally, while progesterone is available in oral form, through an intrauterine device (Mirena IUD), or via vaginal administration. Progesterone is primarily used to safeguard the uterine lining, while estrogen treats symptoms of menopause.
- Dosage of Menopausal Hormone Therapy is customized based on individual symptoms and risk factors. While effective, MHT can slightly increase the risks of blood clots, breast cancer, heart attack, and stroke, particularly in older individuals or those with existing risk factors.
- Starting Menopausal Hormone Therapy is ideally done before age 60 and within 10 years of the last menstrual period. It’s essential to work closely with a healthcare provider to create a personalized treatment plan that balances benefits and risks while monitoring the effectiveness of the therapy.
- Patients can expect to feel the full effects of Menopausal Hormone Therapy within about 12 weeks, with adjustments typically made during follow-up visits. Gradually reducing the dosage may help identify the minimum effective amount, allowing for better management of symptoms while minimizing potential side effects.
Systemic Menopausal Hormone Therapy (MHT) is a widely used method for relieving menopause symptoms, offering significant benefits while also posing potential risks. Estrogen alleviates symptoms, while progesterone protects the uterus. Treatment options include combination therapies and transdermal estrogen, which may reduce the risk of blood clots and cholesterol issues. However, MHT can slightly increase the risk of breast cancer, heart attack, and stroke, especially in older individuals or those with additional risk factors. It’s essential to work with your healthcare provider to develop a personalized treatment plan that effectively balances the benefits and risks of hormone therapy.
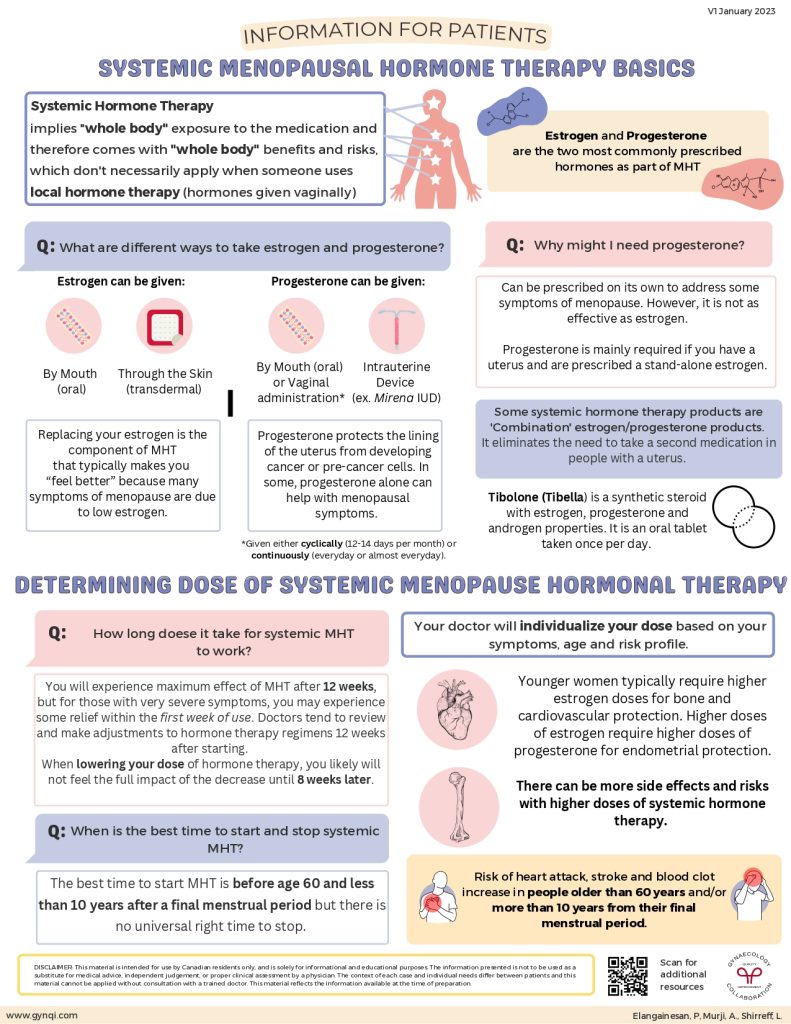
Systemic Menopausal Hormonal Therapy Basics
The term “systemic” denotes the “whole system”, as opposed to talking about a specific part. With systemic hormone therapy, the “whole body” is exposed to the medication and is subjected to both benefits and risks. If you are taking a localized hormone treatment, such as vaginal hormones, the benefits and risks don’t necessarily apply.
As a part of Menopausal Hormone Therapy (MHT), estrogen and progesterone are the two most commonly prescribed hormones.
What are the Different Ways to Take Estrogen and Progesterone?
Many symptoms of menopause are due to low estrogen. Replacing your estrogen is the component of MHT that typically makes you feel better. Estrogen medication can be given:
- By mouth (oral)
- Through the skin (transdermal)
In some cases, progesterone alone can help with menopausal symptoms. Progesterone protects the lining of the uterus from developing cancer or pre-cancer cells. Progesterone can be given:
- By mouth (oral)
- Intrauterine device (Mirena IUD)
- Vaginal administration, given either cyclically (12-14 days per month) or continuously (every day or almost every day).
Why Might I Need Progesterone?
Progesterone can be prescribed on its own to address some symptoms of menopause, however, it is not as effective as estrogen. Progesterone prevents the lining of the uterus from becoming too thick, and is mainly required if you are prescribed a stand-alone estrogen
Combination Therapies
Some systemic hormone therapy products are combination treatments with both estrogen and progesterone. This form of treatment eliminates the need to take a second medication in people with a uterus.
Tibolone (Tibella®) is a synthetic steroid with estrogen, progesterone, and androgen properties. It is an oral tablet taken once per day and is used to treat symptoms that occur when the level of estrogen produced by a woman’s body drops after menopause.
Determining Dose of Systemic Menopause Hormonal Therapy
When starting hormonal therapy, your doctor will tailor your dosage based on your symptoms, age, and risk factors.
Younger women often need higher estrogen doses for bone and heart health, but these higher doses also require increased progesterone for endometrial protection. However, higher doses of systemic hormone therapy can lead to more side effects and risks.
Risks can include:
- Heart attack
- Stroke
- Blood clots
How Long Does it Take for Systemic MHT to Work?
You can expect to feel the full effects of MHT after 12 weeks. However, if your symptoms are very severe, you might notice some relief within the first week.
Doctors typically review and adjust hormone therapy regimens after 12 weeks. If your dose is reduced, it may take up to eight weeks before you feel the full impact of the change.
When is the Best Time to Start and Stop Systemic MHT?
The ideal time to start MHT is before age 60 and within 10 years of your last period. However, there’s no one-size-fits-all answer for when to stop—it’s all about what works best for you.
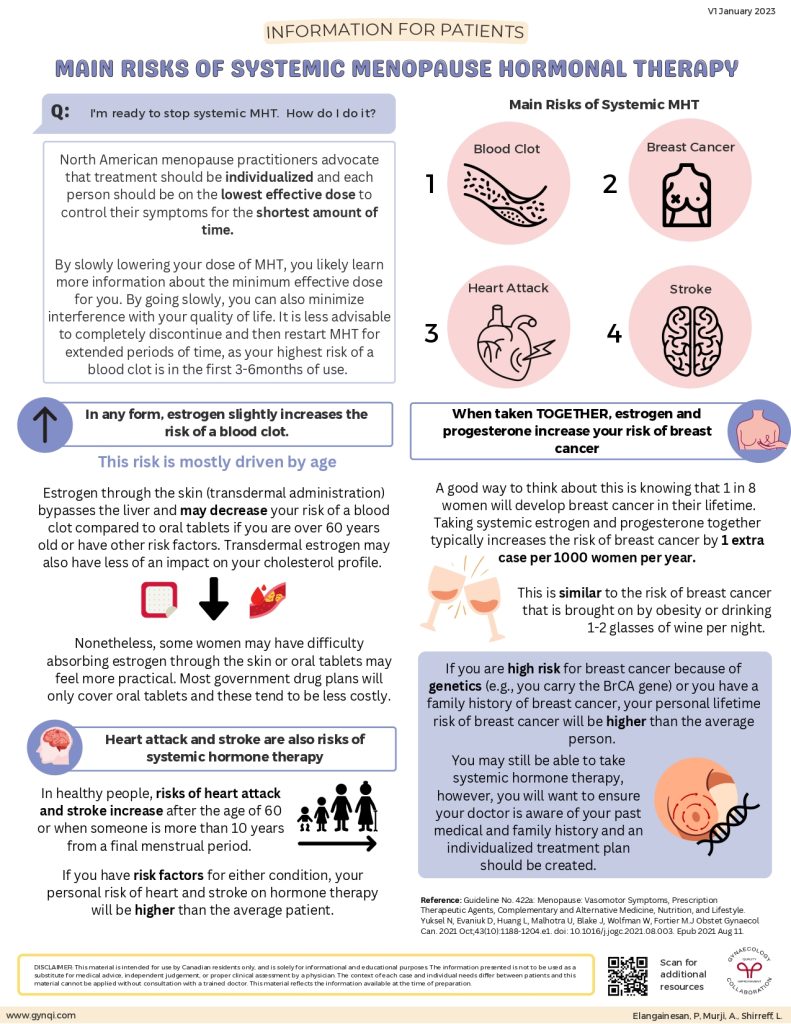
How Do I Stop Taking My Systemic MHT?
Gradually reducing your MHT dose can help you find the minimum effective amount that works for you, while also minimizing interference on your quality of life.
Menopause experts in North America recommend aiming for the lowest effective dose for the shortest time possible to manage symptoms. It’s all about tailoring the plan to each person’s needs.
The Main Risks of Systemic MHT
Blood Clots
Estrogen in any form slightly raises the risk of blood clots, especially in the first three to six months, with age being a major factor. If you are over 60 years old or have other risk factors, transdermal estrogen may lower this risk compared to oral tablets. Transdermal estrogen bypasses the liver, and it may even have less impact on your cholesterol profile.
However, some women have difficulty absorbing estrogen through the skin, and oral tablets are often more affordable and covered by government drug plans.
Breast Cancer
When taken together, estrogen and progesterone can slightly increase the risk of breast cancer.
To put this in a less daunting perspective:
- 1 in 8 women will develop breast cancer in their lifetime
- Using both hormones adds about one extra case per 1,000 women per year
- This risk is similar to the risk from obesity or drinking 1-2 glasses of wine a night
If you have a higher genetic risk, like carrying the BRCA gene or a family history of breast cancer, your personal risk will be greater. In these cases, hormone therapy may still be an option, but it’s important to work with your doctor to create a tailored treatment plan.
Heart-Attack & Stroke
Systemic hormone therapy (MHT) can slightly increase the risk of heart attack and stroke, particularly in individuals over 60 or those more than 10 years past their final menstrual period.
If you have existing risk factors for heart attack or stroke, your personal risk may be higher. It’s important to discuss your medical history with your healthcare provider to determine the most appropriate treatment plan for you.
An Effective Treatment for Managing Menopause Symptoms
Systemic Menopausal Hormone Therapy (MHT) is an effective option for managing menopause symptoms, providing significant relief with estrogen and progesterone. While treatment options like combination therapies and transdermal estrogen may help mitigate some risks, it’s important to remain aware of the potential for increased risks of breast cancer, heart attack, and stroke. Speak with your doctor to find the right treatment plan for you.



