
Table of Contents
- Summary
- What is Vulvar Lichen Planus?
- Subtypes of Vulvar Lichen Planus
- Symptoms of Lichen Planus
- How is Vulvar Lichen Planus Diagnosed?
- Treatment of Vulvar Lichen Planus
- Strong Topical Steroids
- Intralesional Steroid Injections and Oral Steroids
- Alternative Treatments
- Treatment for Vaginal Lichen Planus
- Follow-Up for Lichen Planus
- Keeping Your Vulvar Health in Check
Summary:
- Vulvar Lichen Planus (LP) is a chronic inflammatory condition mostly seen in individuals aged 50 to 60, characterized by painful bumps or sores in moist areas, including the vulva, vagina, and mouth.
- The condition includes several subtypes—such as papulosquamous, erosive, and hypertrophic–each with distinct features. Symptoms can include vaginal burning, soreness, and painful intercourse, with severe cases potentially leading to scar tissue formation.
- Diagnosis typically involves a thorough examination and possible biopsy. While there is no cure, treatments like strong topical steroids, oral medications, and alternative therapies can help manage symptoms and prevent progression.
- Regular follow-up visits are essential to monitor symptoms and assess for any changes in the vulvar skin, as there is a low risk (3-5%) of developing vulvar cancer associated with Lichen Planus.
Vulvar Lichen Planus (LP) is a chronic inflammatory condition commonly affecting individuals aged 50 to 60. It is characterized by painful bumps and sores in moist areas like the vulva, vagina, and mouth, and can present as raw red areas with white lacy patterns, small purple lesions, or erosions extending into the vagina. Although the exact cause remains unclear, it is believed to be an autoimmune disorder. While there is no cure, several treatment options are available to help manage symptoms and prevent the progression of the condition.
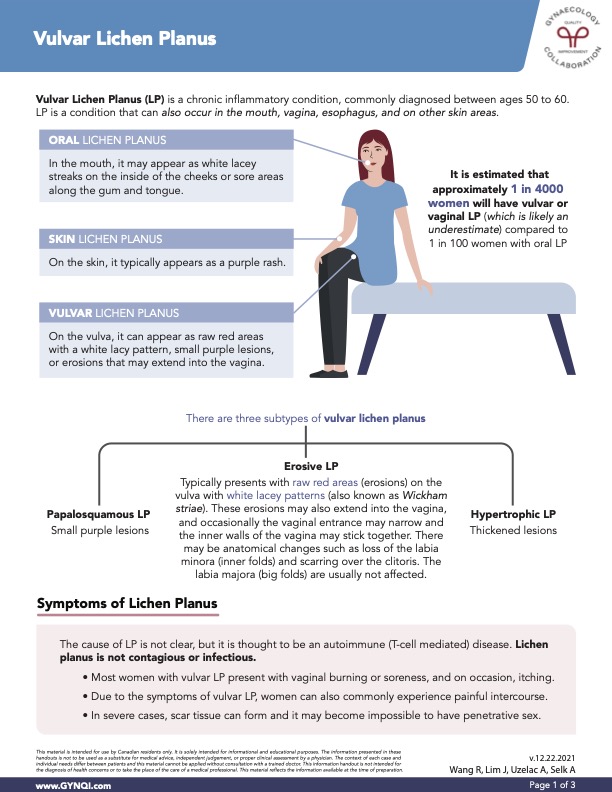
What is Vulvar Lichen Planus?
Vulvar Lichen Planus (LP) is a chronic inflammatory condition, most frequently diagnosed in individuals aged 50 to 60. It is an inflammatory condition marked by bumps or sores in moist areas like the mouth, vagina, esophagus and other skin regions. For most, it is a lifelong condition.
Oral Lichen Planus: It may appear as white lacy streaks on the inside of the cheeks or sore areas along the gum and tongue.
Skin Lichen Planus: Typically appears as a purple rash on the skin.
Vulvar Lichen Planus: Can appear as raw red areas with a white lacy pattern, small purple lesions, or erosions that may extend into the vagina.
Subtypes of Vulvar Lichen Planus
Vulvar Lichen Planus includes several subtypes, each with distinct characteristics and clinical presentations that can influence both diagnosis and treatment options.
Papalosquamous LP: Appears on the vulva as small purple lesions.
Erosive LP: Typically presents as raw red “erosions” on the vulva with white lacy patterns (known as Wickham striae). These erosions can extend into the vagina, potentially causing narrowing at the entrance and adhesion of the inner walls. Anatomical changes can include loss of the labia minora and scarring of the clitoris. The labia majora usually remains unaffected.
Hypertrophic LP: Presents as thickened lesions on the vulva.
Symptoms of Lichen Planus
The exact cause of Lichen Planus remains unclear, though it is believed to be an autoimmune condition mediated by T-cells. Lichen Planus is not contagious or infectious, and transmission is not a concern.
Symptoms can include:
- Vaginal burning or soreness
- Itching (occasionally)
- Painful intercourse
In severe cases, scar tissue can form, making penetrative sex impossible.
How is Vulvar Lichen Planus Diagnosed?
The most important part of diagnosis is a full examination with your doctor. The clinical visit should include a speculum exam (if not too painful) to look inside the vagina. An exam of the inside of the mouth should look for mucosal changes.
A biopsy sample of the vulvar skin can help to establish the diagnosis while ruling out other pre-cancerous lesions, though biopsy results can be non-specific.
Treatment of Vulvar Lichen Planus
While there currently is no cure for vulvar LP, treatments do exist to help manage symptoms and prevent the disease from progressing.
Your first defense is to keep on top of your vulvar care. Stop all possible sources of irritants to the vulva, including avoiding soap and scented products.
Strong Topical Steroids
The first option for treatment is applying strong topical steroids to the vulvar skin. Use of clobetasol or betamethasone diproprionate ointment once to twice per day for three months is typically prescribed.
Contrary to common belief, the use of topical steroids on the vulva is safe and side effects are uncommon when the steroid is used as prescribed. The topical steroid regimen is then tapered and many patients will need to continue on a maintenance therapy.
Intralesional Steroid Injections and Oral Steroids
For more advanced vulvar LP, other routes of steroids may be required. This can include starting oral steroids, or injection of steroids into the vulvar areas with erosions.
Alternative Treatments
If your treatment plan still isn’t effectively managing your symptoms. You can explore alternative treatments with the guidance of your doctor.
These can include:
- Steroid-Sparing Agents: If further treatment is necessary, steroid-sparing agents such as ointments containing calcineurin inhibitors may be recommended. Calcineurin inhibitors are immunosuppressants that effectively manage autoimmune disorders, including conditions of the skin. Tacrolimus or pimecrolimus may be prescribed.
- Oral Treatments: In addition, other oral treatments such as methotrexate, cyclosporin, or mycophenolate mofetil may be used. Additional healthcare providers, usually a dermatologist, are usually involved when starting these oral treatments.
In some cases, vulvar lichen planus does improve on its own and may disappear completely.
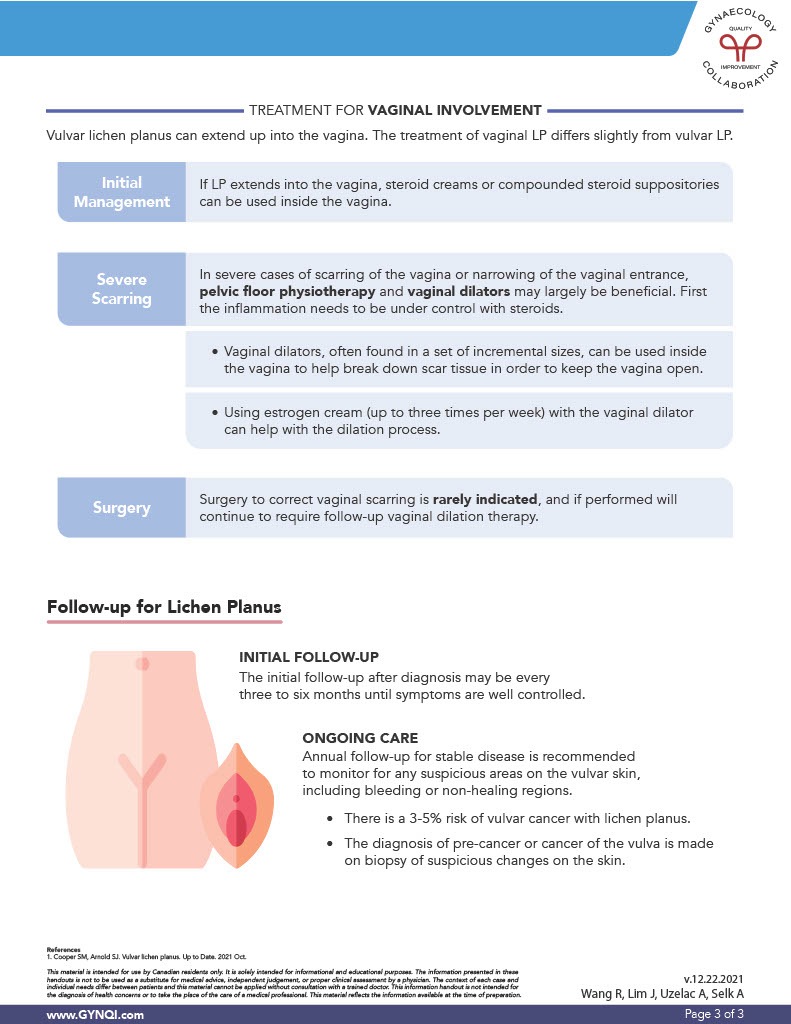
Treatment for Vaginal Lichen Planus
The treatment of vaginal lichen planus differs slightly from vulvar lichen planus. Sometimes, vulvar LP can extend up into the vagina, and a more thorough treatment plan must be taken.
Initial Management: If lichen planus has extended into the vagina, steroid creams or compounded steroid suppositories can be used inside the vagina to stem the progress of symptoms.
Severe Scarring: After inflammation is under control with steroids, approaches like pelvic floor physiotherapy and vaginal dilators may be necessary in severe cases of scarring.
Vaginal dilators are found in a set of incremental sizes and can be used inside the vagina to break down scar tissue and keep the vagina open.
Using an estrogen cream up to three times per week along with the vaginal dilator can help with the dilation process.
Surgery: While surgery to correct vaginal scarring is rare, if performed, vaginal dilation therapy will still be required after surgery.
Follow-Up for Lichen Planus
After diagnosis, follow-up visits with your doctor may be every three to six months until symptoms are managed and under control. For stable disease, an annual check-up is recommended to monitor any suspicious areas on the vulvar skin, especially bleeding or non-healing regions.
While low, there is a 3-5% risk of vulvar cancer with lichen planus. The diagnosis of pre-cancer or cancer of the vulva is made with a biopsy of suspicious changes on the skin. Be sure to let your doctor know immediately if you notice any changes with your vulvar skin.
Keeping Your Vulvar Health in Check
Vulvar Lichen Planus (LP) is a chronic inflammatory condition that presents various symptoms, including painful sores and bumps in moist areas. It can manifest in several distinct subtypes, each requiring specific diagnostic and treatment approaches. While the exact cause remains unclear and although there is currently no cure, effective management strategies—ranging from topical steroids to alternative therapies—can help alleviate symptoms and improve your quality of life. Be sure to follow up regularly with your healthcare provider to monitor the condition and address any concerns you may have.


