Table of Contents
- Summary
- What is Vulvar Lichen Sclerosus?
- Symptoms of Vulvar Lichen Sclerosus
- Discomfort
- Changes to Anatomy
- Functional Changes
- How is Vulvar Lichen Sclerosus Diagnosed?
- Treatment Options for Vulvar Lichen Sclerosus
- Typical Steroid Treatment Plan
- Purpose of Treatment
- Follow-Up for Lichen Sclerosus
- A Proactive Approach to Your Vulvar Health
Summary:
- Vulvar Lichen Sclerosus (LS) is a chronic inflammatory condition primarily affecting the vulvar skin and impacts about 1% of women, often diagnosed around menopause but possible at any age.
- Common symptoms include severe itching, burning, and pain during intercourse, along with potential anatomical changes like pale and fragile skin, scarring, and a narrowing of the vaginal opening.
- Diagnosis typically involves a clinical examination and possibly a skin biopsy, while treatment focuses on ongoing management with topical steroids, with options like oral steroids and immunomodulators available for persistent cases.
- Regular follow-ups are crucial to monitor symptoms and prevent further complications, including the approximately 5% risk of progression to vulvar cancer if lichen sclerosus remains untreated.
Vulvar Lichen Sclerosus (LS) is a chronic inflammatory condition affecting the vulva, primarily impacting around 1% of women who are often diagnosed around menopause. Though its exact cause is unclear, it may involve autoimmune factors and a genetic predisposition to the disease. Common symptoms include itching, burning, and anatomical changes that can disrupt normal vulvar function. Upon diagnosis, regular follow-ups are crucial to monitor for potential complications, including a risk of vulvar cancer.
What is Vulvar Lichen Sclerosus?
Vulvar Lichen Sclerosus (LS) is a long-term inflammatory condition that targets the genital skin, especially the vulva. Around 1% of women experience LS, and most diagnoses happen around menopause, though it can occur at any age. In up to 15% of cases, it can also pop up in other skin areas.
While the exact cause is still a bit of a mystery, it is thought to have an autoimmune component, and with a genetic link as it is found more often in families. Vulvar Lichen Sclerosus doesn’t affect the vagina.
Symptoms of Vulvar Lichen Sclerosus
It can be a lot to navigate, but understanding the changes can help!
Discomfort
The most common symptoms of LS include:
- Itching
- Burning
- Pain during sexual intercourse
The itching can become severe, and with persistent scratching, this can lead to cuts that are painful.
Changes to Anatomy
Lichen Sclerosus can occur anywhere on the vulva and perianal skin, and can also cause changes to anatomy. Over time, affected skin can become pale, thin, and develop white patches. This skin becomes fragile and can crack.
In more advanced cases, the disease can alter the normal vulvar anatomy, causing scarring, loss of labia minora (the ”inner lips”), fusion over the clitoris, and narrowing of the vaginal opening.
Functional Changes
As a result of any anatomical changes, many individuals can experience a disruption of normal function as a result. This can include:
- Inability to properly urinate
- Painful sexual intercourse
- Painful bowel movements
How is Vulvar Lichen Sclerosus Diagnosed?
Diagnosis of LS is often made based on your symptoms and an examination of the skin around the vulva and anus.
A skin biopsy is sometimes required to confirm a diagnosis of LS. The biopsy can often be performed in an office setting under local freezing, with the small sample of the skin then sent to the laboratory for examination. For a skin biopsy to be accurate, any steroids applied to the skin should be avoided on the vulva for at least four weeks beforehand.
Treatment Options for Vulvar Lichen Sclerosus
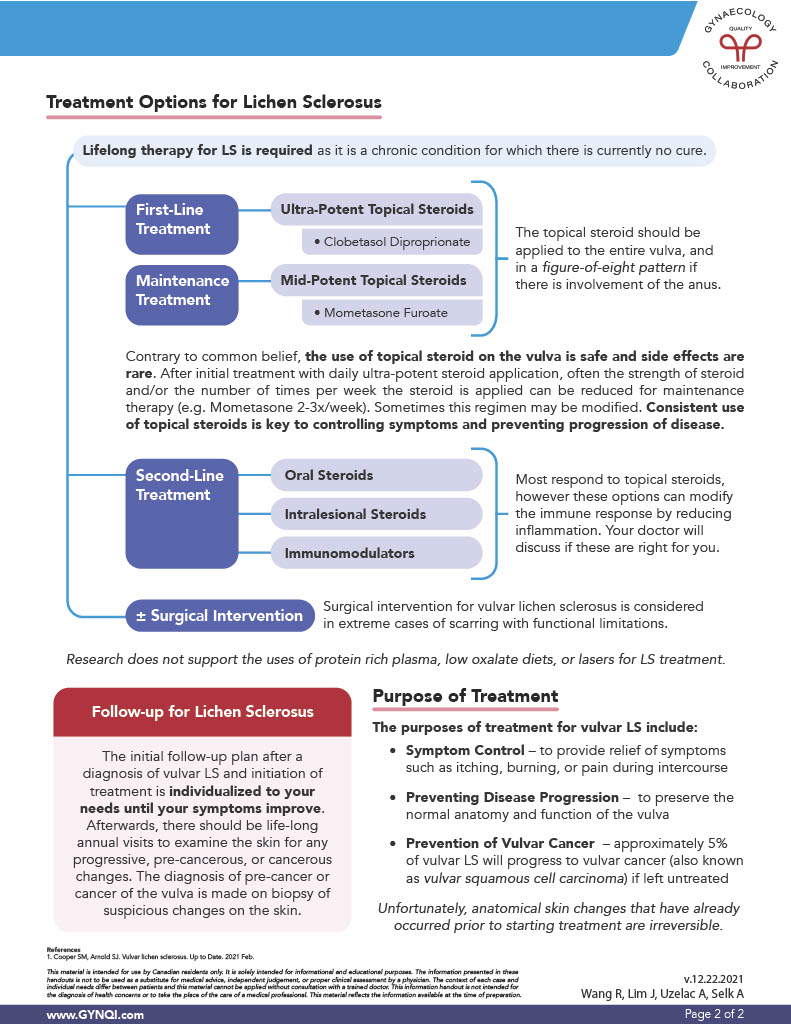
Managing Lichen Sclerosus requires ongoing treatment as it is a chronic condition for which there is currently no cure. Steroids may be used in order to keep symptoms and disease progression under control.
Contrary to common belief, the use of topical steroids on the vulva is safe and side effects are rare. The topical steroid should be applied to the entire vulva, and in a figure-eight pattern if the anus is affected.
Typical Steroid Treatment Plan
Consistent use of topical steroids is key to controlling your symptoms and preventing the progression of the disease. If symptoms persist, further steroid treatment options can be explored.
First Line of Treatment: Ultra-potent topical steroids such as Clobetasol Diproprionate will be prescribed.
Maintenance Treatment: After starting with ultra-potent steroids, the next step is to reduce the strength or frequency of steroid application for maintenance therapy (e.g. Mometasone 2-3 times a week). This regimen can be adjusted as needed.
Second-Line Treatment: Most respond to topical steroids, but if extra help is needed, the following treatment options can modify the immune response by reducing inflammation.
- Oral Steroids – synthetic hormones taken by mouth to treat LS
- Intralesional Steroids – corticosteroids injected directly into lesions to reduce inflammation
- Immunomodulators – oral tablets or injections that modify the immune system’s response, either by enhancing or suppressing its activity. Your doctor will discuss if these options are right for you.
- Surgical Intervention – While rare, in cases of scarring and changes to vulva anatomy and function, surgery may be required.
Currently, research does not support the use of protein-rich plasma treatments, low-oxalate diets, or laser therapy.
Purpose of Treatment
A treatment plan should be implemented to include:
- Symptom control and management of painful symptoms such as itching, burning, or pain during intercourse.
- Preventing disease progression and preserving the normal anatomy and function of the vulva.
- Prevention of vulvar cancer. Approximately 5% of vulvar lichen sclerosus will progress to vulvar cancer (vulvar squamous cell carcinoma) if left untreated.
Unfortunately, anatomical skin changes that have already occurred before starting treatment are irreversible.
Follow-up for Lichen Sclerosus
After a diagnosis of vulvar lichen sclerosus, the follow-up plan and initiation of treatment are tailored to your needs until your symptoms improve. Afterward, there should be life-long annual check-ups to examine the skin for any progressive, precancerous, or cancerous changes. The diagnosis of pre-cancer or cancer of the vulva is made with a biopsy of suspicious changes on the skin.
A Proactive Approach to Your Vulvar Health
Vulvar Lichen Sclerosus is a chronic inflammatory condition that impacts the vulvar skin, leading to discomfort and potential irreversible anatomical changes. While its exact cause is currently unknown, understanding the symptoms is vital for effective management. Ongoing treatment with topical steroids is essential to control symptoms and prevent progression, including the risk of vulvar cancer if untreated. Regular follow-up appointments are crucial for monitoring changes and ensuring appropriate care. Speak to your doctor if you notice any changes of concern to your vulva and surrounding areas.


