Table of Contents
- Summary
- Introduction
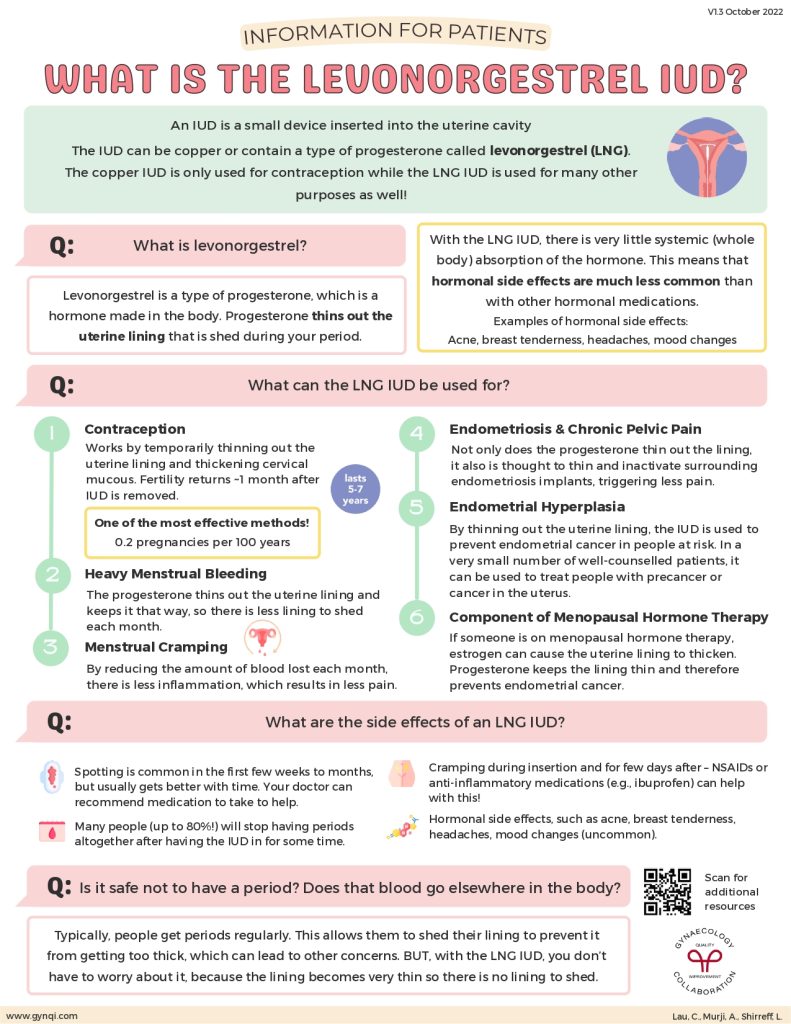
- What Is the Levonorgestrel IUD?
- What is Levonorgestrel?
- When Should You Consider the Levonorgestrel IUD?
- Contraception
- Heavy Menstrual Bleeding
- Endometriosis & Chronic Pain
- Endometrial Hyperplasia
- Menopausal Hormone Therapy
- Side Effects of Levonorgestrel IUD
- Is Not Having a Period Safe?
- Who Should NOT Use the LNG IUD?
Summary:
- The Levonorgestrel IUD, or intrauterine device, delivers a steady dose of hormones directly to the uterus. This provides effective contraception and reduces the thickness of the uterine lining for up to five years at a time.
- Levonorgestrel is a progestin, a type of hormone naturally produced in the body that helps to regulate the menstrual cycle. When delivered via an IUD, it can help to reduce symptoms like painful periods or heavy bleeding.
- The LNG IUD is very well-tolerated by most patients, but may trigger mild side effects like headaches or nausea in some women. These symptoms often self-resolve without any intervention.
- Levonorgestrel may reduce the frequency of periods or stop them altogether. This is completely safe, and occurs because progestins prevent the lining of the uterus from developing in the first place.
- You shouldn’t use levonorgestrel and/or an IUD if you are pregnant, planning to become pregnant, have cancer, or have an active infection. If you plan to have surgery or are scheduled for imaging, you should let your care team know you have an IUD in advance.
The Levonorgestrel IUD can be a safe and effective way to prevent pregnancy and treat certain hormonal conditions, including heavy or painful periods. Unlike many oral birth control pills, it is estrogen-free and only works in the uterus itself, rather than affecting the entire body.
If you’re looking for long-term contraception or are struggling with uncomfortable symptoms like painful periods, the LNG IUD may be able to help. Ask your doctor whether this progestin-based hormone device is right for you.
What is the Levonorgestrel IUD?
An IUD (Intrauterine Device) is a small, T-shaped device that is inserted into the uterus to prevent pregnancy or control symptoms related to certain hormonal conditions. Once placed, they provide long-term, fully reversible contraception for anywhere between 3 to 10 years.
There are two main types of IUDs:
- Copper IUDs: Non-hormonal IUDs like Liberté, FlexiT, and Monalisa are made from copper. They slowly release copper ions into the uterus over time, which acts like a spermicide and prevents fertilization.
- Hormone IUDs: Hormonal IUDs are made from a hollow plastic frame that comes pre-loaded with hormones—typically progestin. These devices thicken cervical mucus and thin the uterine lining, preventing ovulation, fertilization, and implantation.
The Levonorgestrel IUD (LNg) is a form of hormonal IUD. It steadily releases hormones over time to prevent pregnancy, but may also reduce heavy periods, lessen the intensity of menstrual cramps, or reverse abnormal growth of the uterine lining.
What is Levonorgestrel?
Levonorgestrel is a synthetic form of progesterone, a natural hormone produced by the body at varying points in the menstrual cycle. It works by signaling the body to prevent ovulation, thicken cervical mucus, and reduce the thickness of the uterine lining.
The LNG IUD delivers a consistent dose of levonorgestrel directly to the uterus, and that’s where most of the medication stays. Only a tiny amount of the hormone is absorbed into the bloodstream, which greatly lowers your risk for side effects like weight gain, nausea, and breast tenderness.
When Should You Consider the Levonorgestrel IUD?
Your doctor will work closely with you to determine if the Levonorgestrel IUD is right for you. You will usually have a pap smear and/or imaging to assess your risk for potential side effects or contraindications before they approve insertion. Doctors typically recommend this device in the following situations.
Contraception
The Levonorgestrel IUD is one of the most effective and reversible methods of contraception currently available. It has a failure rate of just 0.2% and fertility often returns within around 1 month after removal.
Heavy Menstrual Bleeding
Levonorgestrel thins out the uterine lining and keeps it that way, so there is less lining to shed each month. That usually results in lighter periods—or in some cases, no periods at all!
Menstrual Cramping
A thinner uterine lining means less blood loss each month, which also reduces period-related inflammation. Some women may notice a reduction in period pain as a result.
Endometriosis & Chronic Pelvic Pain
Levonorgestrel affects all endometrial tissue, including both the uterine lining and any endometriosis implants located elsewhere in the body. It may help to reduce any related pain.
Endometrial Hyperplasia
The Levonorgestrel IUD thins the lining of the uterus, which may also help to reduce the risk of abnormal cell growth. In a small number of well-counseled patients, it can also be used to treat precancerous cells or early-stage endometrial cancer.
Menopausal Hormone Therapy
If someone is on menopausal hormone therapy, estrogen can cause the uterine lining to thicken. Progesterone keeps the lining thin, which may prevent the development of endometrial cancers.
It can be helpful to make a list of why you’re considering an IUD and any questions you have about it before you visit the doctor. Don’t be afraid to ask questions while you’re there—it’s important to be informed before you move forward.
Side Effects of the Levonorgestrel IUD
The Levonorgestrel IUD is generally well-tolerated by patients. In fact, most women never experience any side effects at all over the life of their device. A small number of people do report problems like:
- Spotting: Common in the first few weeks to months, spotting usually gets better with time. Your doctor can recommend medication to help.
- Amenorrhea: Many people (up to 80%!) will stop having periods altogether after having the IUD in for some time.
- Cramping: It’s common to have cramping during insertion or even for a few days after. NSAIDs or anti-inflammatory medications (e.g., ibuprofen) can help with this!
- Hormonal Side Effects: Although it is extremely uncommon, some women might experience side effects like acne, breast tenderness, headaches, or mood changes.
For patients who do experience side effects, symptoms tend to be mild at often self-resolve over time. However, you should still tell your doctor about problems like breakthrough bleeding, cramping, acne, headaches, or nausea right away.
Is Not Having a Period Safe?
Generally, yes. If you’ve heard that not having your period is unhealthy or can lead to cancer and fertility problems, this is likely a result of confusion between amenorrhea from progestins and a more serious but fairly common hormone condition.
Most people have a period once every 21 to 28 days, which allows the uterine lining to shed. When this doesn’t happen, the lining (called the endometrium) can become too thick or even develop precancerous cells. This is called endometrial hyperplasia.
The Levonorgestrel IUD prevents the endometrium from developing or greatly slows how fast it grows. Because there’s little to no lining to shed, endometrial hyperplasia is much less likely to occur. In fact, doctors sometimes use levonorgestrel to slow or reverse the growth of abnormal cells that may eventually lead to endometrial cancer.
Who Should NOT Use the LNG IUD?
Some people shouldn’t use the Levonorgestrel or the LNG IUD. This product is contraindicated in patients who are/have:
- Pregnant or planning to become pregnant
- Pelvic Inflammatory Disease (PID)
- An active gynecologic infection (e.g., bacterial vaginosis)
- An untreated sexually transmitted infection (e.g., chlamydia)
- Certain gynecologic cancers (e.g., cervical cancer)
- Advanced liver disease (e.g., cirrhosis or liver failure)
You should also let your care team know that you have an IUD before having surgery, a CT scan, an MRI, or an ultrasound. While having an IUD usually isn’t a contraindication, it may affect imaging results or require your surgeon to modify their approach, especially during procedures like fibroid revision or hysterectomy.



