Table of Contents
- Summary
- Vasomotor Symptoms of Menopause
- Treatment Options for Vasomotor Symptoms
- Lifestyle Modifications
- Non-Prescription Treatments
- Non-Hormonal Prescription Drugs
- Menopause Hormone Therapy (MHT)
- Contraindications to Menopause Hormone Therapy
- Taking Charge of Your Well-Being
Summary:
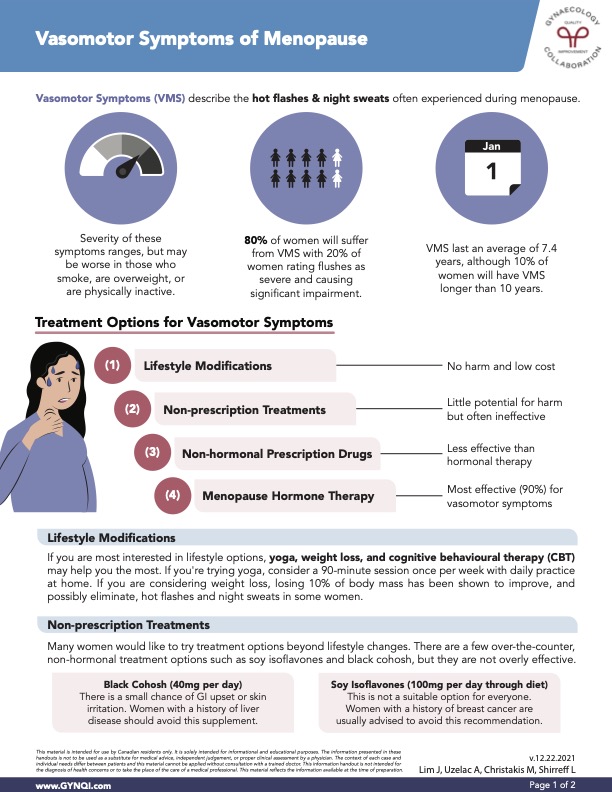
- Hot flashes and night sweats affect approximately 80% of women during menopause, with 20% experiencing severe symptoms that disrupt daily life. VMS typically lasts an average of 7.4 years, but for some, it can persist for over a decade.
- Effective low-cost strategies for managing VMS include yoga, weight loss, and cognitive behavioural therapy (CBT). A 10% reduction in body weight can reduce or eliminate symptoms for some women.
- Over-the-counter non-hormonal remedies like soy isoflavones and black cohosh often have limited effectiveness. Non-hormonal prescription options, such as low-dose antidepressants and gabapentin, can be considered but are generally less effective than hormone therapy.
- MHT is the most effective treatment for VMS, providing relief for 90% of women. It’s essential to discuss potential risks and contraindications with your doctor to create a personalized treatment plan that maximizes benefits and minimizes risks.
- Before starting MHT, it’s crucial to discuss any potential risks with your doctor, especially if you have a history of unexplained vaginal bleeding, breast or endometrial cancer, severe liver disease, coronary heart disease, and more.
Vasomotor Symptoms (VMS), including hot flashes and night sweats, affect around 80% of women during menopause. Their severity can be worsened by factors like smoking, excess weight, and physical inactivity, with symptoms lasting an average of 7.4 years for some women. Fortunately, several treatment options exist, including lifestyle modifications, non-prescription treatments, and Menopause Hormone Therapy (MHT). Each option has its unique benefits and considerations, so it’s important to discuss them with your doctor to determine the most suitable plan for your needs.
Vasomotor Symptoms of Menopause
Vasomotor Symptoms (VMS) refer to the hot flashes and night sweats that many women experience during menopause. The intensity of these symptoms varies, with factors like smoking, excess weight, and lack of physical activity potentially worsening them. Around 80% of women will encounter VMS, and for 20%, these episodes can be so severe that they disrupt daily life. On average, VMS lasts an average of 7.4 years, but for 10% of women, these symptoms can persist for over a decade.
Treatment Options for Vasomotor Symptoms
When it comes to managing vasomotor symptoms, there are several treatment options available that can help reduce the intensity and frequency of hot flashes and night sweats.
Lifestyle Modifications
For a low-cost, no-harm approach, lifestyle changes like yoga, weight loss, and cognitive behavioural therapy (CBT) can be effective. A weekly 90-minute yoga session, with daily at-home practice, can offer relief. If you are considering weight loss, it has been shown that a 10% reduction in body weight can reduce or even eliminate hot flashes and night sweats for some women.
Non-Prescription Treatments
Though many women seek alternatives to lifestyle changes, over-the-counter non-hormonal options like soy isoflavones and black cohosh often have little effect and limited success. They do, however, pose a risk, although it’s minimal.
- Black Cohosh (40mg per day): There is a small chance of gastrointestinal upset or skin irritation. Women with a history of liver disease should avoid this supplement.
- Soy Isoflavones (100mg per day through diet): This is not a suitable option for everyone. Women with a history of breast cancer are usually advised to avoid this option.
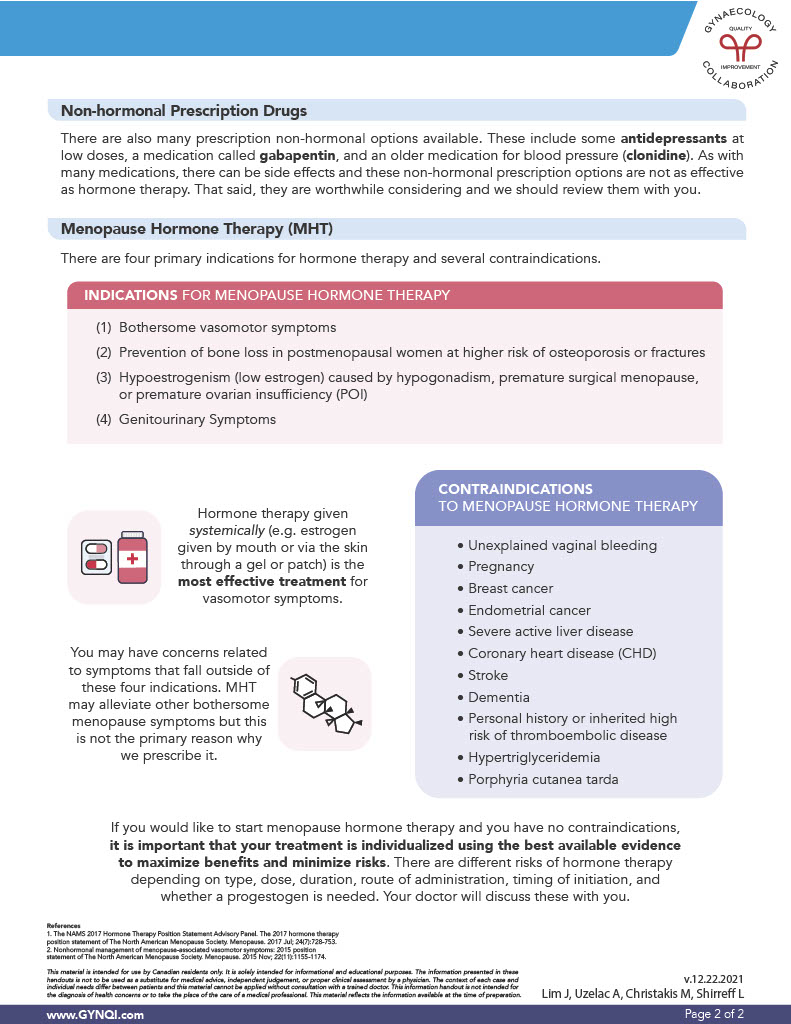
Non-Hormonal Prescription Drugs
Several non-hormonal prescription options are available, including low-dose antidepressants, gabapentin, and an older blood pressure medication called clonidine. While less effective than hormone therapy and with potential side effects, these treatments are still worth considering and should be reviewed with your doctor.
Menopause Hormone Therapy (MHT)
Menopause Hormone Therapy (MHT) is the most effective treatment for vasomotor symptoms, providing relief for 90% of women. It is primarily used for four key indications:
- Bothersome vasomotor symptoms
- Prevention of bone loss in postmenopausal women at a higher risk of osteoporosis or fractures
- Hypoestrogenism (low estrogen) caused by hypogonadism, premature surgical menopause, or premature ovarian insufficiency (POI)
- Genitourinary symptoms
Hormone therapy given systemically (e.g. estrogen taken orally or via the skin through a gel or patch) is the most effective treatment for vasomotor symptoms.
You may have concerns related to symptoms that fall outside of these four indications, and while MHT may alleviate other bothersome symptoms, these four indications are the primary reason they are prescribed.
Contraindications to Menopause Hormone Therapy
With menopause hormone therapy, there are several potential risks that should be carefully considered. Speak to your doctor if you have a history of any of the following:
- Unexplained vaginal bleeding
- Pregnancy
- Breast cancer
- Endometrial cancer
- Severe active liver disease
- Coronary heart disease (CHD)
- Stroke
- Dementia
- Personal history or inherited high risk of thromboembolic disease
- Hypertriglyceridemia
- Porphyria cutanea tarda
Taking Charge of Your Well-Being
If you’re considering menopause hormone therapy and have no contraindications, it’s essential that your treatment is personalized based on the best available evidence to maximize benefits and minimize risks. The risks of hormone therapy vary depending on factors like the type, dose, duration, administration method, timing of initiation, and whether there is a need for progestogen. Your doctor will guide you through these considerations.
By tailoring your treatment plan to your specific needs, you can feel confident that you’re making the best choice for your long-term health and well-being.



