Table of Contents
- Summary
- Introduction
- What is MHT?
- A Quick Note On Progesterone First
- Local Hormone Therapy
- Systemic Hormone Therapy
- Systemic MHT Risks
- Breast Cancer
- Stroke
- Heart Attack
- Blood Clot
- Systemic MHT Risks
- Assessing Your Level of Risk
- Who Shouldn’t Use MHT?
- New MHT Medications
- Duavive
- Tibella
Summary:
- As women approach menopause, estrogen levels drop. This can produce a constellation of uncomfortable symptoms, like hot flashes and Genitourinary Syndrome of Menopause (GSM), that significantly impact the quality of life.
- Menopause Hormone Therapy, or MHT, can help women get effective relief. These products are available in both oral and local formats.
- Most treatments contain estrogen and/or progesterone. Currently, hormones like these are the most effective treatment for symptoms of menopause on the market.
- Systemic hormones (e.g., oral pills) are generally safe, but may slightly raise your risk for strokes, heart attacks, blood clots, and breast cancers. Local therapies (e.g., insertable creams or suppositories) can help reduce these risks without sacrificing relief.
What is MHT?
Menopause Hormone Therapy (MHT) refers to treating symptoms associated with menopause, like hot flashes, insomnia, and vaginal dryness, with estrogen and/or progesterone. As a woman approaches and enters this chapter of her life, natural estrogen levels begin to drop, which can trigger uncomfortable symptoms that significantly impact her quality of life.
Estrogen is the most effective treatment available on the market in Canada. It may be prescribed as an oral pill, topical gel, insertable ring, or insertable cream.
Why is Menopause Hormone Therapy Prescribed?
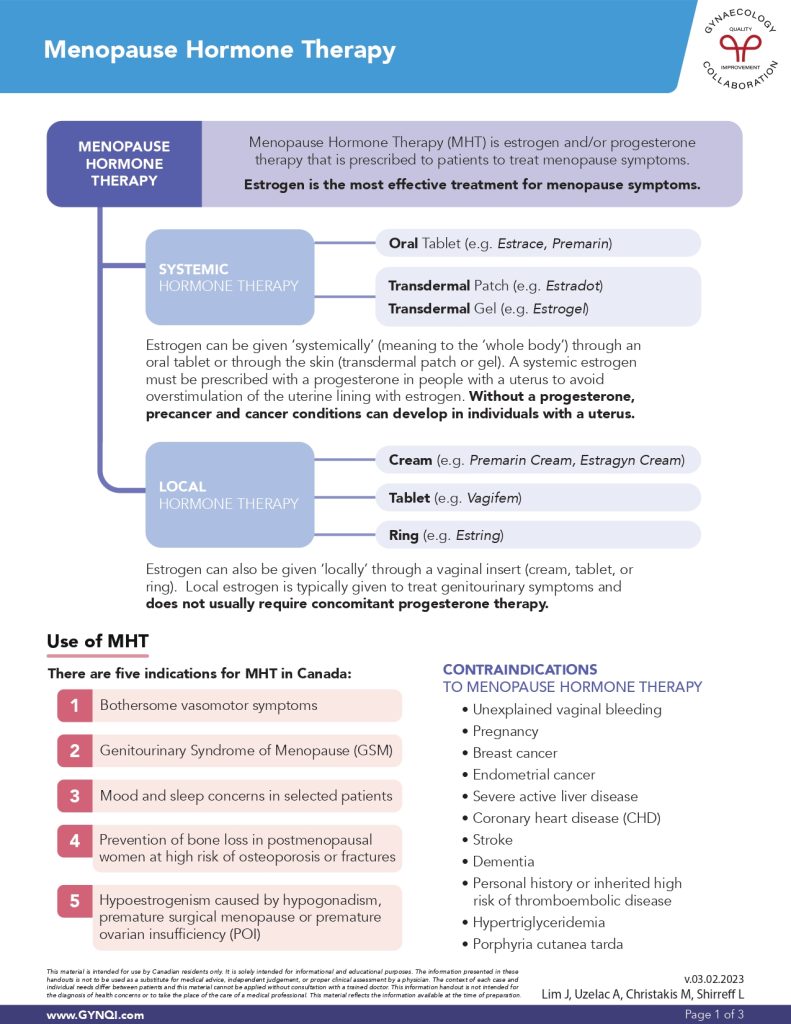
There are five main indications for MHT in Canada:
- Bothersome vasomotor symptoms, including sweating or hot flashes.
- Genitourinary Syndrome of Menopause (GSM), including sexual dysfunction.
- Mood and sleep concerns, including anxiety or insomnia.
- Bone loss prevention, especially in women at risk for osteoporosis or fractures
- Hypoestrogenism caused by hypogonadism, premature surgical menopause, or premature ovarian insufficiency (POI)
If you’re suffering from one of these conditions, are in menopause, or are approaching menopause, ask your doctor if MHT is right for you.
A Quick Note On Progesterone First
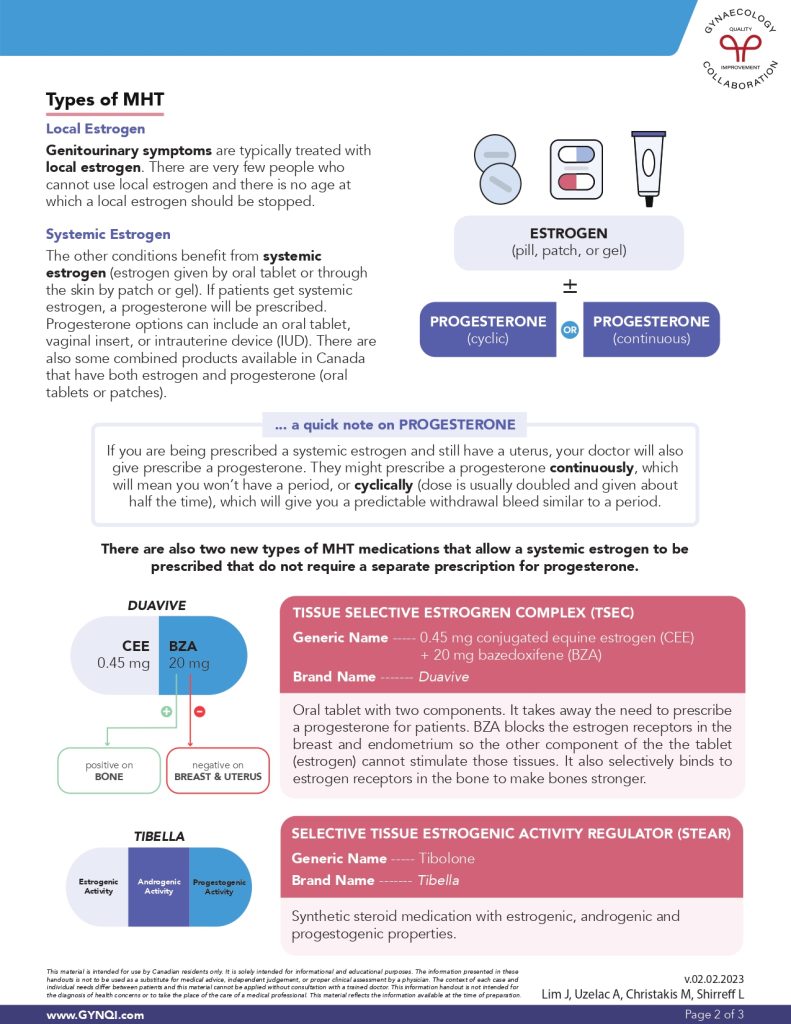
If you are being prescribed systemic estrogen and still have a uterus, your doctor will also prescribe progesterone. They might prescribe progesterone continuously, which will mean you won’t have a period, or cyclically (the dose is usually doubled and given about half the time), which will give you a predictable withdrawal bleed similar to a period.
Local Hormone Therapy
Genitourinary symptoms like vaginal dryness, atrophy, and sexual dysfunction respond best to local estrogen therapy. There are very few people who cannot use local estrogen and there is no age at which a local estrogen should be stopped.
Local hormone therapies are available as a:
- Cream (e.g., Premarin Cream, Estragyn Cream)
- Tablet (e.g., Vagifem)
- Ring (e.g., Estring)
Local estrogen does not usually require concomitant progesterone therapy, as only a tiny amount of hormone is absorbed into the bloodstream. This greatly reduces your risk for problems typically associated with oral pills, including heart attacks, blood clots, and strokes.
Systemic Hormone Therapy
Patients who suffer from symptoms of menopause that are unrelated to GSM often get more effective relief from systemic estrogen (meaning to the “whole body”) estrogens. These are typically prescribed as an oral tablet, transdermal patch, or gel.
- Oral Tablet (e.g., Estrace, Premarin)
- Transdermal Patch (e.g., Estradot)
- Transdermal Gel (e.g., Estrogel)
If you still have your uterus, your provider will likely prescribe progesterone to take alongside estrogen-based treatments. It is extremely important to continue taking this second medication unless your doctor tells you to stop, as an excess of estrogen alone can rarely trigger the growth of precancerous cells or cancers in the uterus.
Progesterone options can include:
- An oral tablet (e.g., Jencycla, Norlutate)
- A vaginal insert (e.g, Endometrin)
- An intrauterine device (IUD) (e.g., Mirena)
Combination products with estrogen and progesterone are available in Canada. These contain both hormones in a single oral tablet or patch.
Systemic MHT Risks
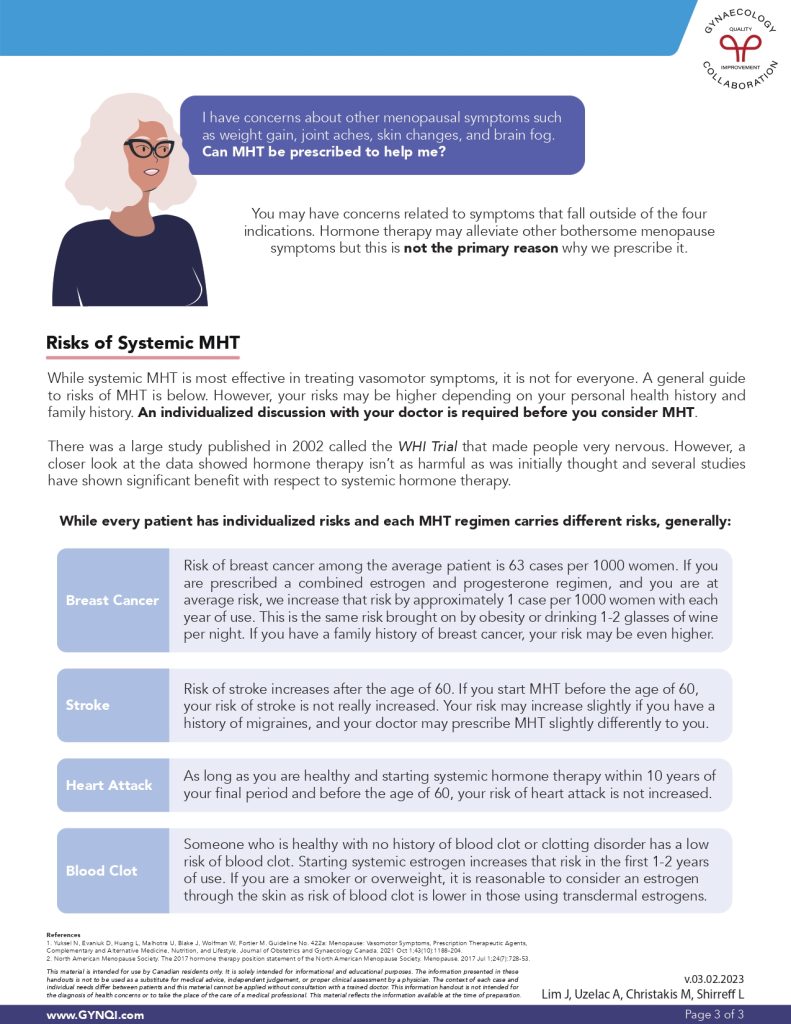
Systemic MHT is the most effective option for treating vasomotor symptoms like hot flashes, but up until a few years ago, many providers were hesitant to prescribe it. Their concerns stemmed from a large study published in 2002 called the WHI Trial, which made people very nervous about potential side effects.
A closer look at the data later showed that hormone therapy wasn’t as harmful as initially thought. In fact, the results of several studies since then have suggested that MHT might actually provide other indirect health benefits beyond symptom management alone.
Your doctor can help walk you through your personal health profile so you can decide whether systemic hormones are right for you. In general, the most serious risks fall into one of the following four categories.
Breast Cancer
The risk of breast cancer among the average patient is 63 cases per 1,000 women. If you are prescribed a combined estrogen and progesterone regimen, and you are at average risk, the risk increases by approximately 1 case per 1,000 women with each year of use. This is the same risk brought on by obesity or drinking 1-2 glasses of wine per night.
If you have a family history of breast cancer, your risk may be even higher. Your doctor may determine that oral tablets aren’t right for you, but local therapies might still be an option.
Stroke
Women over the age of 60 have an elevated baseline risk for strokes, and there is evidence to suggest that starting MHT after this age may further increase that risk. Starting hormone therapy before this point in time doesn’t have the same effect.
Your risk for a stroke may also be heightened if you have a history of migraines. Your doctor may change how they prescribe MHT or adapt your treatment to address these concerns.
Heart Attack
As long as you are healthy and starting systemic hormone therapy within 10 years of your final period—and before the age of 60—your risk of having a heart attack remains the same. You may be unable to use MHT if you have certain pre-existing cardiac conditions.
Blood Clot
Someone who is healthy with no history of blood clots or clotting disorders has a low risk of blood clots in the first place. Starting systemic estrogen does slightly increase that risk in the first 1-2 years after you begin MHT.
If you are a smoker or overweight, it is reasonable to consider estrogen through the skin rather than oral pills. Your risk of blood clots is much lower when using transdermal estrogens.
Assessing Your Level Of Risk
Determining your personal level of risk starts with having a frank conversation with your provider. They can help you review your personal health history, medications, and family history to identify whether MHT is right for you.
Who Shouldn’t Use MHT?
Some patients shouldn’t use MHT or may need to stop using MHT if they begin experiencing undesirable side effects. While every patient is unique, the most common contraindications usually include:
- Unexplained vaginal bleeding
- Pregnancy
- Breast cancer
- Endometrial cancer
- Severe active liver disease
- Coronary heart disease (CHD)
- Stroke
- Dementia
- Personal history or inherited high risk of thromboembolic disease
- Hypertriglyceridemia
- Porphyria cutanea tarda
If you’re already on MHT, tell your doctor right away if you have or experience one of these symptoms. They may want to change your treatment plan or adjust your dose.
New MHT Medications
There are also two new types of MHT medications that allow systemic estrogen to be prescribed that do not require a separate prescription for progesterone. Both are only available as an oral pill.
Duavive
Duavive is a Tissue Selective Estrogen Complex (TSEC). Each oral tablet contains 0.45 mg conjugated equine estrogen (CEE) and 20 mg bazedoxifene (BZA).
BZA blocks the estrogen receptors in the breast and endometrium so the other component of the tablet—estrogen—cannot stimulate those tissues. It also selectively binds to estrogen receptors in your bones to help make them stronger.
Tibella
Tibella (tibolone) is a Selective Tissue Estrogenic Activity Regulator (STEAR) that doesn’t contain any actual hormones. Instead, it is a synthetic steroid medication that breaks down into three substances that mimic estrogen, progesterone, and testosterone in the body.
Menopause Doesn’t Have to Hold You Back
If you’re struggling with menopause symptoms, it’s important to know that you don’t have to suffer in silence. There are many hormone therapy options available that are suitable for different patient symptoms, preferences, and risk factors. Ask your doctor if one of these options can help restore your quality of life.



