Table of Contents
- Summary
- Introduction
- What Causes GSM?
- Symptoms of GSM
- Non-Pharmacologic Treatments
- Pharmacological Treatments
- Non-Hormonal Options
- Hormonal Pharmacological Options
- Local Estrogens
- Ospemifene (Osphena)
- Special Information About Breast Cancer
Summary:
- Genitourinary Syndrome of Menopause (GSM) is a condition that occurs in some women after menopause as estrogen levels drop. Vagina and genital tissues may become dry, fragile, or thin.
- GSM can cause a wide variety of symptoms ranging from chronic pain to frequent urinary tract infections and sexual dysfunction. New treatments can help you get relief from the condition and prevent it from worsening over time.
- Treatments may involve taking medication, using oral hormone pills, or applying hormones locally to vaginal tissues. Or, they may be more holistic in nature and focus on helping relieve symptoms without medication.
- Oral estrogens can pose a risk to patients who have had breast cancer or who are being treated for it currently. However, local products may be an acceptable alternative.
Genitourinary Syndrome of Menopause (GSM) is very common and can impair quality of life, sexual function, and relationships with partners. Without adequate and timely treatment, it can eventually evolve into a chronic concern that results in longstanding functional and structural changes in the urogenital tissues.
While GSM can be difficult to reverse once these changes happen, there are excellent options available to help treat symptoms and prevent them from worsening over time.
What Causes GSM?
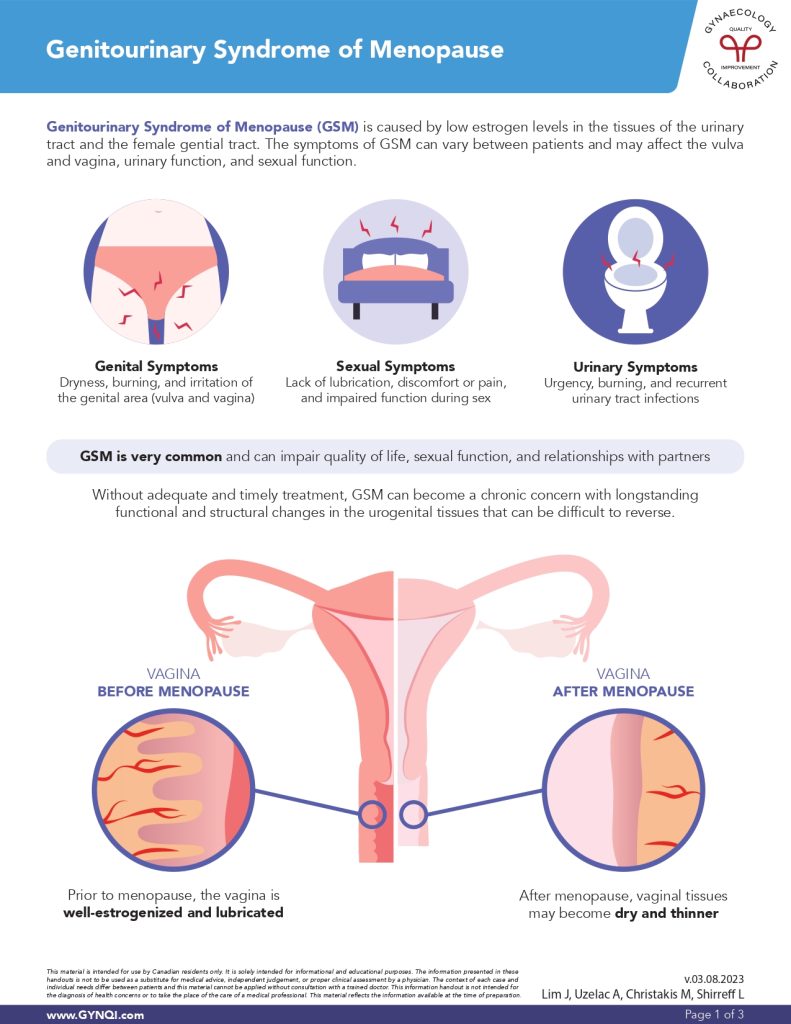
GSM is caused by low estrogen levels in the tissues of the urinary tract and the female genital tract. Before menopause, the vagina is well supplied with estrogens that keep tissues supple, elastic, and lubricated. After menopause, estrogen levels fall, which can cause tissues to become thin or dry.
Symptoms of GSM
The symptoms of GSM can vary between patients and may affect the vulva and vagina, urinary function, and sexual function.
- Genital Symptoms: Dryness, burning, and irritation of the genital area.
- Urinary Symptoms: Urgency, burning, and recurrent urinary tract infections.
- Sexual Symptoms: Lack of lubrication, discomfort, pain, or impaired sexual function.
Because every patient is unique, the way people cope with all of these symptoms can vary widely. They may be mildly irritating for some, but completely overwhelming for others. All experiences are valid and should be factored into treatment plans.
Non-Pharmacologic Treatments
The symptoms of GSM are very real and not just “in your head.” However, approaching treatment holistically, with a focus on the mind-body connection, can be highly beneficial for some women. This is especially true if your symptoms cause a significant amount of anxiety or stress, which can inadvertently worsen GSM.
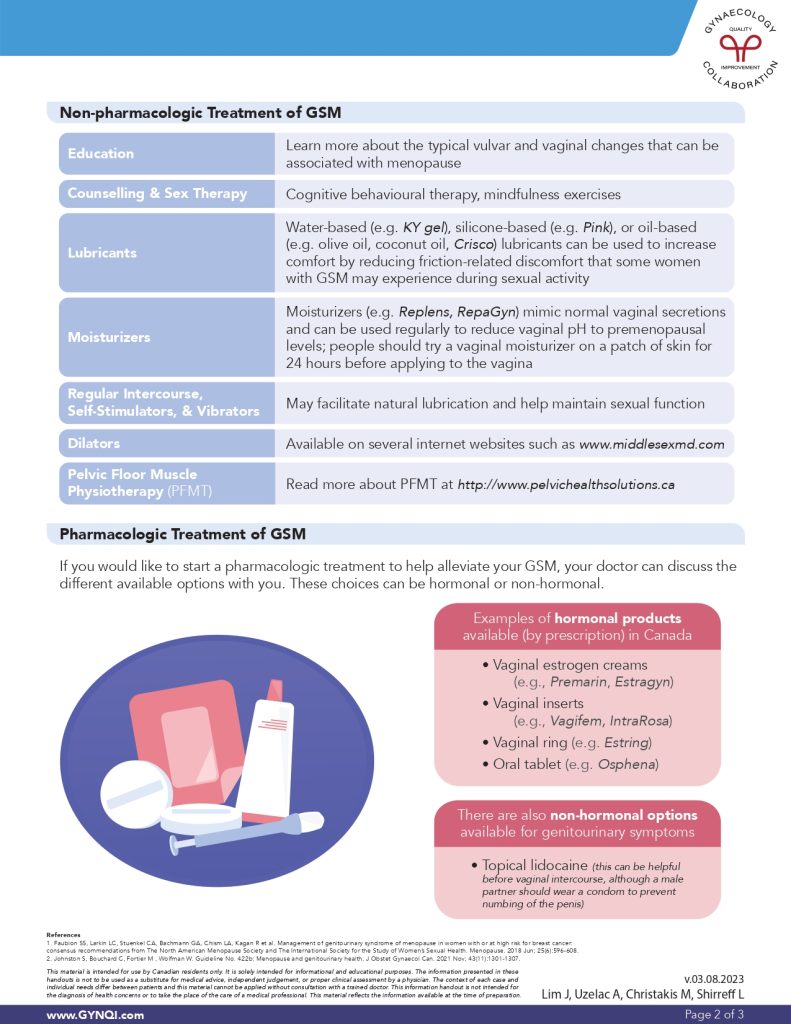
- Education: Learn more about the typical vulvar and vaginal changes that can be associated with menopause. Knowledge is power!
- Counselling & Sex Therapy: Cognitive behavioural therapy and mindfulness exercises can help you cope with systems and restore lost intimacy.
- Lubricants: Water-based (e.g. KY gel), silicone-based (e.g. Pink), or oil-based (e.g. olive oil, coconut oil, Crisco) lubricants can be used to increase comfort and reduce friction during sex.
- Moisturizers: Moisturizers (e.g. Replens, RepaGyn) mimic normal vaginal secretions and can be used regularly to reduce vaginal pH to premenopausal levels. Try a vaginal moisturizer on an external patch of skin for 24 hours before applying it to the vagina.
- Regular Intercourse, Self-Stimulators, & Vibrators: Self-pleasure can help facilitate natural lubrication and maintain sexual function.
- Dilators: Dilators are tube-shaped devices in varying sizes that may help some patients maintain vaginal depth and width. They’re available online from MiddleSexMD.
- Pelvic Floor Muscle Physiotherapy (PFMT): Pelvic floor dysfunction can play a role in GSM. Special physiotherapies may help restore function— read more about it at Pelvic Health Solutions.
Pharmacologic Treatments for GSM
Pharmacological treatments can help reduce the symptoms of GSM and prevent it from further developing as you age. These choices can be hormonal or non-hormonal—your doctor can walk you through the available options if you’re curious about them.
Non-Hormonal Treatments for GSM
Some pharmacological treatments for GSM focus on managing symptoms without the need for topical or oral hormones. The most common options are:
- Topical Lidocaine can also be applied before intercourse to help with discomfort, although male partners should wear a condom to prevent numbing of the penis.
- Laser Therapy can provide relief for some patients, and is approved by Health Canada for the treatment of GSM.
Hormonal Pharmacologic Options for GSM
Hormones are the most commonly diagnosed treatments available on the market for GSM and the symptoms associated with it. Most of these products are applied “locally” rather than taken by mouth. Ospemifene, an oral pill, is sometimes recommended by doctors for GSM.
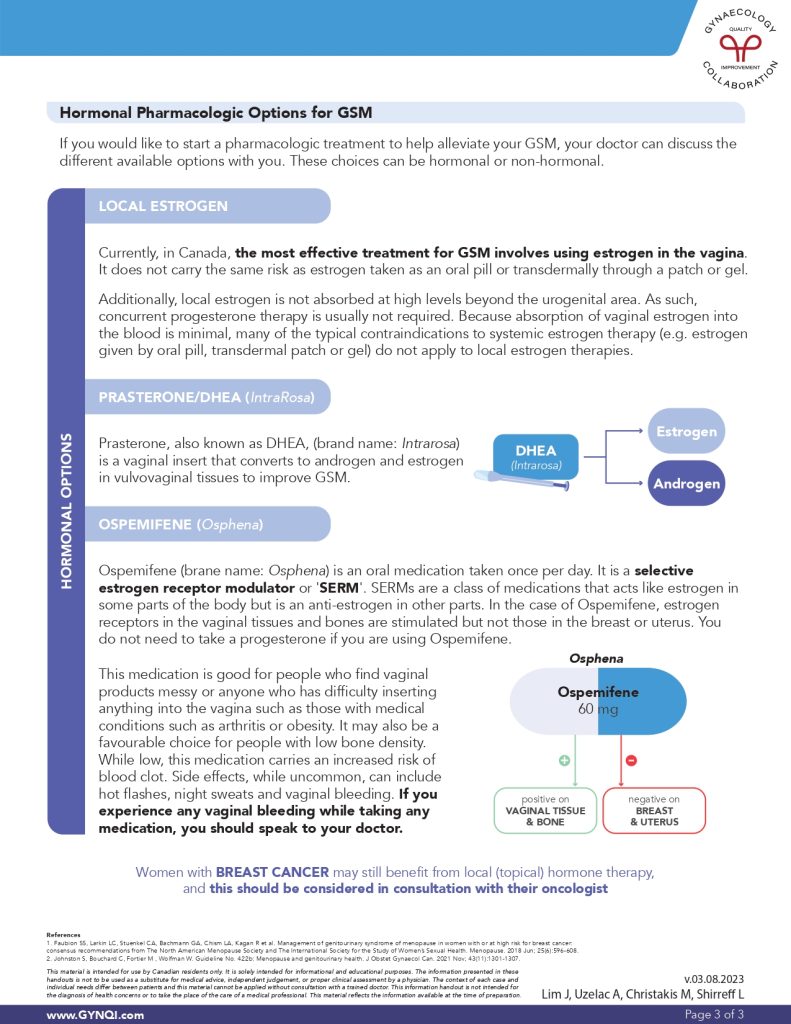
Local Estrogens
The most effective treatment for GSM involves using estrogen in the vagina, which does not carry the same risks as systemic estrogen. Local estrogen isn’t absorbed into the bloodstream at high levels beyond the immediate urogenital area. For this reason, concurrent progesterone therapy is not usually required.
- Vaginal estrogen creams: (e.g., Premarin, Estragyn)
- Vaginal inserts: (e.g., Vagifem, IntraRosa)
- Vaginal ring: (e.g., Estring)
- Prasterone, also known as DHEA, is a special vaginal insert that converts to both androgen and estrogen in vulvovaginal tissues.
Most of these products come with an applicator device to help you insert the product. Some, like Vagifem, come individually loaded in the applicator for easier use.
Ospemifene (Osphena)
Ospemifene (brand name: Osphena) is an oral medication taken once per day. It is a selective estrogen receptor modulator, or ‘SERM’.
- Ospemifene activates estrogen receptors in the vaginal tissues and bones but doesn’t have the same effect on the breasts or uterus.
- You may not need to take progesterone if you are using Ospemifene.
- Ospemifene may be a good option for people who find vaginal products messy or who struggle to insert products into the vagina.
- It is often recommended for people with low bone density.
While the risk is very low, ospemifene does carry an increased risk for blood clots. Other side effects associated with it include:
- Hot flashes
- Night sweats
- Vaginal bleeding
If you experience any vaginal bleeding while taking any medication, even if it is temporary and stops on its own, speak to your doctor right away.
Special Information About Hormones and Breast Cancer
Some hormones, including estrogen, may pose a risk to patients who are at an increased risk for breast cancer, have had breast cancer in the past, or are currently being treated for it. If this is the case for you, make sure your care team is aware of your history before starting any hormone-based treatments—even those applied locally.
Women with BREAST CANCER may still benefit from local (topical) hormone therapy but should be closely monitored by an oncologist.
Reclaim Your Quality Of Life
If the symptoms of GSM are impacting your quality of life, know that there are many options out there. Non-pharmacologic and pharmacologic non-hormonal and hormonal options for treatment exist to help prevent and alleviate your symptoms. Ask your doctor if one of these options is right for you.



